Psoriasis is an inflammatory skin condition where immune cells play a significant role. The importance of the cross-talk between keratinocytes and immune cells in the pathogenesis of psoriasis has recently been reaffirmed. Recent studies have found that several S1PR functional antagonists, other than S1PR2, are effective in improving psoriasis. This study aims to investigate the role of S1PR2 in psoriasis, that has not been investigated before.
Spatial transcriptomics, RT-qPCR, and flow cytometry were used to map the immune cell landscape and its association with metabolic pathways in an imiquimod (IMQ)-induced psoriasis-like inflammation in S1pr2fl/fl K14-Cre mice that could not sense sphingosine-1-phosphate (S1P) in the epidermis through the S1PR2 receptor.
Our analysis suggests that S1PR2 in keratinocytes plays a major role in psoriasis-like inflammation compared to other S1PRs. It acts as a down-regulator, inhibiting the recruitment of Th17 cells into the skin. In IMQ-induced psoriasis skin, both S1pr2-/- and S1pr2fl/fl K14-Cre mice showed higher expressions of proinflammatory cytokines such as TNF-α, IL-17A, and IL-1β together with higher expressions of MyD88/NF-κB pathway compared to the wild-type mice. Remarkably, in IMQ-treated mice, the deletion of S1pr2 in keratinocytes only resulted in a larger population of Th17 cells in skin-draining lymph nodes. Other S1PR modulators did not improve the worsening of psoriasis-like inflammation caused by S1PR2 deficiency in keratinocytes.
This study reaches two main conclusions: signals from keratinocytes play a central role in creating an immune environment that promotes the development of psoriasis, and stimulating S1PR2, instead of suppressing it, represents a potential therapeutic approach for psoriasis.
Copyright © 2024 Masuda-Kuroki, Alimohammadi, Lowry and Di Nardo.
In Frontiers in Immunology on 11 October 2024 by Masuda-Kuroki, K., Alimohammadi, S., et al.
In Cell Communication and Signaling : CCS on 30 September 2024 by Fang, C., Ren, P., et al.
Mitochondria play a crucial role in shaping the macrophage inflammatory response during bacterial infections. Spinster homolog 2 (Spns2), responsible for sphingosine-1-phosphate (S1P) secretion, acts as a key regulator of mitochondrial dynamics in macrophages. However, the link between Spns2/S1P signaling and mitochondrial functions remains unclear.
Peritoneal macrophages were isolated from both wild-type and Spns2 knockout rats, followed by non-targeted metabolomics and RNA sequencing analysis to identify the potential mediators through which Spns2/S1P signaling influences the mitochondrial functions in macrophages. Various agonists and antagonists were used to modulate the activation of Spns2/S1P signaling and its downstream pathways, with the underlying mechanisms elucidated through western blotting. Mitochondrial functions were assessed using flow cytometry and oxygen consumption assays, as well as morphological analysis. The impact on inflammatory response was validated through both in vitro and in vivo sepsis models, with the specific role of macrophage-expressed Spns2 in sepsis evaluated using Spns2flox/floxLyz2-Cre mice. Additionally, the regulation of mitochondrial functions by Spns2/S1P signaling was confirmed using THP-1 cells, a human monocyte-derived macrophage model.
In this study, we unveil prostaglandin E2 (PGE2) as a pivotal mediator involved in Spns2/S1P-mitochondrial communication. Spns2/S1P signaling suppresses PGE2 production to support malate-aspartate shuttle activity. Conversely, excessive PGE2 resulting from Spns2 deficiency impairs mitochondrial respiration, leading to intracellular lactate accumulation and increased reactive oxygen species (ROS) generation through E-type prostanoid receptor 4 activation. The overactive lactate-ROS axis contributes to the early-phase hyperinflammation during infections. Prolonged exposure to elevated PGE2 due to Spns2 deficiency culminates in subsequent immunosuppression, underscoring the dual roles of PGE2 in inflammation throughout infections. The regulation of PGE2 production by Spns2/S1P signaling appears to depend on the coordinated activation of multiple S1P receptors rather than any single one.
These findings emphasize PGE2 as a key effector of Spns2/S1P signaling on mitochondrial dynamics in macrophages, elucidating the mechanisms through which Spns2/S1P signaling balances both early hyperinflammation and subsequent immunosuppression during bacterial infections.
© 2024. The Author(s).
In EBioMedicine on 1 April 2024 by Dinh, D. D., Wan, H., et al.
In male mice, a circadian rhythm in myogenic reactivity influences the extent of brain injury following subarachnoid haemorrhage (SAH). We hypothesized that female mice have a different cerebrovascular phenotype and consequently, a distinct SAH-induced injury phenotype.
SAH was modelled by pre-chiasmatic blood injection. Olfactory cerebral resistance arteries were functionally assessed by pressure myography; these functional assessments were related to brain histology and neurobehavioral assessments. Cystic fibrosis transmembrane conductance regulator (CFTR) expression was assessed by PCR and Western blot. We compared non-ovariectomized and ovariectomized mice.
Cerebrovascular myogenic reactivity is not rhythmic in females and no diurnal differences in SAH-induced injury are observed; ovariectomy does not unmask a rhythmic phenotype for any endpoint. CFTR expression is rhythmic, with similar expression levels compared to male mice. CFTR inhibition studies, however, indicate that CFTR activity is lower in female arteries. Pharmacologically increasing CFTR expression in vivo (3 mg/kg lumacaftor for 2 days) reduces myogenic tone at Zeitgeber time 11, but not Zeitgeber time 23. Myogenic tone is not markedly augmented following SAH in female mice and lumacaftor loses its ability to reduce myogenic tone; nevertheless, lumacaftor confers at least some injury benefit in females with SAH.
Female mice possess a distinct cerebrovascular phenotype compared to males, putatively due to functional differences in CFTR regulation. This sex difference eliminates the CFTR-dependent cerebrovascular effects of SAH and may alter the therapeutic efficacy of lumacaftor compared to males.
Brain Aneurysm Foundation, Heart and Stroke Foundation and Ted Rogers Centre for Heart Research.
Copyright © 2024 The Author(s). Published by Elsevier B.V. All rights reserved.
In Hepatology Communications on 1 March 2024 by Islam, D., Israr, I., et al.
Ductular reactivity is central to the pathophysiology of cholangiopathies. Mechanisms underlying the reactive phenotype activation by exogenous inflammatory mediators and bile acids are poorly understood.
Using human extrahepatic cholangiocyte organoids (ECOs) we developed an injury model emulating the cholestatic microenvironment with exposure to inflammatory mediators and various pathogenic bile acids. Moreover, we explored roles for the bile acid activated Sphingosine-1-phosphate receptor 2 (S1PR2) and potential beneficial effects of therapeutic bile acids UDCA and norUDCA.
Synergistic exposure to bile acids (taurocholic acid, glycocholic acid, glycochenodeoxycholic acid) and TNF-α for 24 hours induced a reactive state as measured by ECO diameter, proliferation, lactate dehydrogenase activity and reactive phenotype markers. While NorUDCA and UDCA treatments given 8 hours after injury induction both suppressed reactive phenotype activation and most injury parameters, proliferation was improved by NorUDCA only. Extrahepatic cholangiocyte organoid stimulation with S1PR2 agonist sphingosine-1-phosphate reproduced the cholangiocyte reactive state and upregulated S1PR2 downstream mediators; these effects were suppressed by S1PR2 antagonist JET-013 (JET), downstream mediator extracellular signal-regulated kinase 1/2 inhibitor, and by norUDCA or UDCA treatments. JET also partially suppressed reactive phenotype after bile acid injury.
We developed a novel model to study the reactive cholangiocyte state in response to pathological stimuli in cholestasis and demonstrated a contributory role of S1PR2 signaling in both injury and NorUDCA/UDCA treatments. This model is a valuable tool to further explore the pathophysiology of human cholangiopathies.
Copyright © 2024 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of the American Association for the Study of Liver Diseases.
In IScience on 21 April 2023 by Fukuzaki, Y., Faustino, J., et al.
Arterial ischemic stroke is common in neonates-1 per 2,300-5,000 births-and therapeutic targets remain insufficiently defined. Sphingosine-1-phosphate receptor 2 (S1PR2), a major regulator of the CNS and immune systems, is injurious in adult stroke. Here, we assessed whether S1PR2 contributes to stroke induced by 3 h transient middle cerebral artery occlusion (tMCAO) in S1PR2 heterozygous (HET), knockout (KO), and wild type (WT) postnatal day 9 pups. HET and WT of both sexes displayed functional deficits in Open Field test whereas injured KO at 24 h reperfusion performed similarly to naives. S1PR2 deficiency protected neurons, attenuated infiltration of inflammatory monocytes, and altered vessel-microglia interactions without reducing increased cytokine levels in injured regions at 72 h. Pharmacologic inhibition of S1PR2 after tMCAO by JTE-013 attenuated injury 72 h after tMCAO. Importantly, the lack of S1PR2 alleviated anxiety and brain atrophy during chronic injury. Altogether, we identify S1PR2 as a potential new target for mitigating neonatal stroke.
© 2023 The Authors.
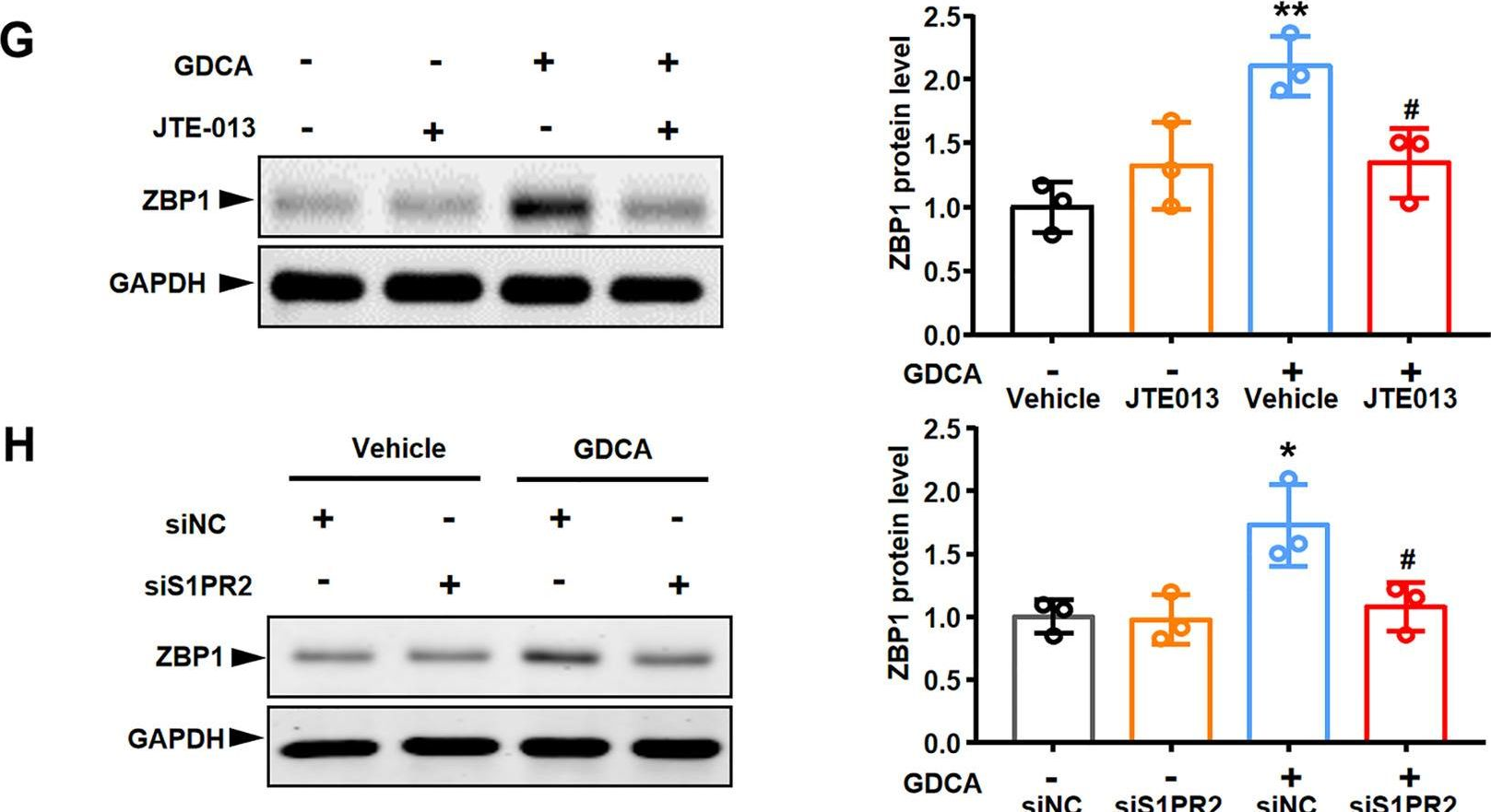
In Cell Death Dis on 1 March 2023 by Yang, S., Chang, N., et al.
Fig.7.G
-
WB
-
Collected and cropped from Cell Death & Disease by CiteAb, provided under a CC-BY license
Image 1 of 1
