The skin is constantly exposed to environmental sensory stimuli, which may include harmful volatiles and small hydrophobic molecules. However, the skin's protective mechanism against the latter agents is unclear. Here, we demonstrate that odorant binding protein 2A (OBP2A) protects epidermal keratinocytes against cytotoxic small hydrophobic molecules. OBP2A is mainly expressed in human epidermal keratinocytes. Cellular resistance to cytotoxic aldehyde and lipids was reduced in keratinocytes when OBP2A was silenced. Furthermore, silencing of OBP2A in a three-dimensional epidermal equivalent model resulted in impairment of epidermal barrier function. Inhibition of OBP2A caused disruption of keratinocyte lipid metabolism and induced endoplasmic reticulum stress. OBP2A expression was markedly decreased in the epidermis of atopic dermatitis lesional skin. In addition, interleukin-13 suppressed the expression of OBP2A in keratinocytes. Overall, our findings suggest that OBP2A regulates epidermal barrier function and contributes to protection of the skin against harmful small hydrophobic molecules.
© 2024 The Author(s).
In IScience on 15 November 2024 by Nakanishi, S., Hasegawa, T., et al.
In Scientific Reports on 17 January 2022 by Iriyama, S., Ogura, Y., et al.
The epidermal basement membrane deteriorates with aging. We previously reported that basement membrane reconstruction not only serves to maintain epidermal stem/progenitor cells in the epidermis, but also increases collagen fibrils in the papillary dermis. Here, we investigated the mechanism of the latter action. Collagen fibrils in the papillary dermis were increased in organotypic human skin culture treated with matrix metalloproteinase and heparinase inhibitors. The expression levels of COL5A1 and COL1A1 genes (encoding collagen type V α 1 chain and collagen type I α 1 chain, respectively) were increased in fibroblasts cultured with conditioned medium from a skin equivalent model cultured with the inhibitors and in keratinocytes cultured on laminin-511 E8 fragment-coated plates. We then examined cytokine expression, and found that the inhibitors increased the expression of PDGF-BB (platelet-derived growth factor consisting of two B subunits) in epidermis. Expression of COL5A1 and COL1A1 genes was increased in cultured fibroblasts stimulated with PDGF-BB. Further, the bifunctional inhibitor hydroxyethyl imidazolidinone (HEI) increased skin elasticity and the thickness of the papillary dermis in the skin equivalent. Taken together, our data suggests that reconstructing the basement membrane promotes secretion of PDGF-BB by epidermal keratinocytes, leading to increased collagen expression at the papillary dermis.
© 2022. The Author(s).
In Scientific Reports on 28 July 2020 by Iriyama, S., Yasuda, M., et al.
Daily sunlight exposure damages the epidermal basement membrane (BM) and disrupts epidermal homeostasis. Inter-follicular epidermal stem cells (IFE-SCs) regulate epidermal proliferation and differentiation, which supports epidermal homeostasis. Here, we examine how photoaging affects the function of IFE-SCs and we identify key components in their cellular environment (niche). We found that sun-exposed skin showed a decrease of MCSP-positive and β1-integrin-positive cells concomitantly with a decrease of laminin-511 at the dermal-epidermal junction (DEJ), as compared with sun-protected skin. Higher levels of laminin-511 were associated with not only increased efficiency of colony formation, but also higher expression levels of MCSP as well as other stem cell markers such as Lrig1, ITGB1, CD44, CD46, DLL1, and K15 in keratinocytes from skin of 12- to 62-year-old subjects. UVB exposure to cultured human skin impaired laminin-511 integrity at the dermal-epidermal junction and reduced MCSP-positive basal epidermal cells as well as K15-positive cells. Combined treatment with matrix metalloproteinase and heparanase inhibitors protected the integrity of laminin-511 and inhibited the reduction of MCSP-positive cells and K15-positive cells. These results suggest that photoaging may reduce the levels of MCSP-positive and K15-positive epidermal stem/progenitor cells in the epidermis via loss of laminin-511 at the dermal-epidermal junction.
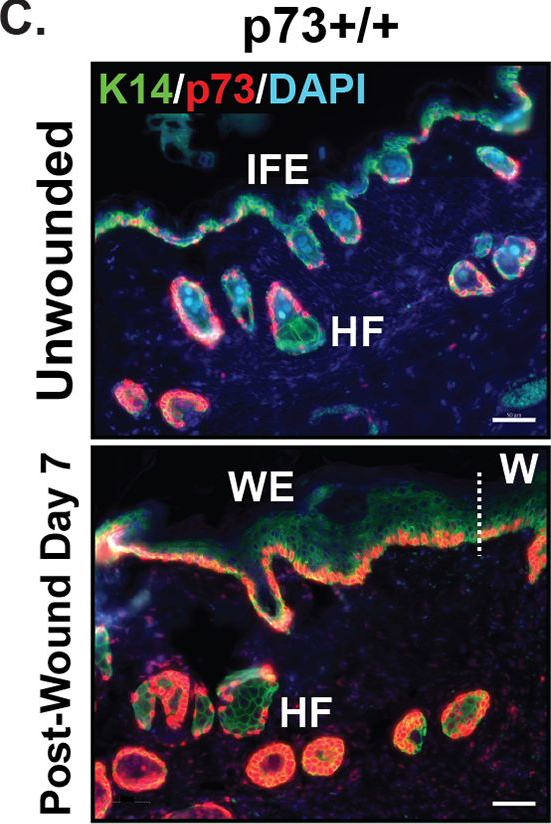
p73 regulates epidermal wound healing and induced keratinocyte programming.
In PLoS ONE on 20 June 2019 by Beeler, J. S., Marshall, C. B., et al.
p63 is a transcriptional regulator of ectodermal development that is required for basal cell proliferation and stem cell maintenance. p73 is a closely related p53 family member that is expressed in select p63-positive basal cells and can heterodimerize with p63. p73-/- mice lack multiciliated cells and have reduced numbers of basal epithelial cells in select tissues; however, the role of p73 in basal epithelial cells is unknown. Herein, we show that p73-deficient mice exhibit delayed wound healing despite morphologically normal-appearing skin. The delay in wound healing is accompanied by decreased proliferation and increased levels of biomarkers of the DNA damage response in basal keratinocytes at the epidermal wound edge. In wild-type mice, this same cell population exhibited increased p73 expression after wounding. Analyzing single-cell transcriptomic data, we found that p73 was expressed by epidermal and hair follicle stem cells, cell types required for wound healing. Moreover, we discovered that p73 isoforms expressed in the skin (ΔNp73) enhance p63-mediated expression of keratinocyte genes during cellular reprogramming from a mesenchymal to basal keratinocyte-like cell. We identified a set of 44 genes directly or indirectly regulated by ΔNp73 that are involved in skin development, cell junctions, cornification, proliferation, and wound healing. Our results establish a role for p73 in cutaneous wound healing through regulation of basal keratinocyte function.
In Experimental Dermatology on 1 March 2019 by Iriyama, S., Yamanishi, H., et al.
Daily exposure to sunlight is known to affect the structure and function of the epidermal basement membrane (BM), as well as epidermal differentiation and epidermal barrier function. The aim of this study is to clarify whether the inhibition of BM-degrading enzymes such as heparanase and matrix metalloproteinase 9 (MMP-9) can improve the epidermal barrier function of facial skin, which is exposed to the sun on a daily basis. 1-(2-hydroxyethyl)-2-imidazolidinone (HEI) was synthesized as an inhibitor of both heparanase and MMP-9. HEI inhibited not only the BM damage at the DEJ but also epidermal proliferation, differentiation, water contents and transepidermal water loss abnormalities resulting from ultraviolet B (UVB). This was determined in this study by the use of UVB-induced human cultured skins as compared with the control without HEI. Moreover, topical application of HEI improved epidermal barrier function by increasing water content and decreasing transepidermal water loss in daily sun-exposed facial skin as compared with non-treated skins. These results suggest that the inhibition of both heparanase and MMP-9 is an effective way to care for regularly sun-exposed facial skin by protecting the BM from damage.
© 2019 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd.
In PLoS One on 20 June 2019 by Beeler, J. S., Marshall, C. B., et al.
Fig.2.C
-
IHC-IF
-
Mus musculus (House mouse)
Collected and cropped from PLoS ONE by CiteAb, provided under a CC-BY license
Image 1 of 1
