The introduction of checkpoint immunotherapeutic agents in the last decade has revolutionized cancer treatment. Although anti-PD-1, anti-PD-L1 and anti-CTLA4 are promising therapies, many patients fail to respond or relapse due to drug resistance potentially due to redundancy of immune checkpoints. One of the ways to improve the efficacy of this cancer treatment is to target two or even three immune checkpoints. To date, the benefit of combined anti-VISTA/anti-PD-L1 therapy has been confirmed, but no one has investigated the efficacy of blocking these negative immune checkpoints with a bispecific anti-VISTA/anti-PD-L1 antibody.
In this study, the bispecific antibodies (bsAbs) were produced in three formats: symmetric (IgG-HC-scFv), asymmetric (Fab-scFv-Fc(KIH)) and 2 x scFv. The binding and blocking properties of these bispecific antibodies (bsAbs) and their efficacy compared to monotherapy and combination therapy were then determined using endometrial (RL95-2), pancreatic (PANC-1) and breast (BT-20) cancer cell lines.
The bsAbs generated in this study showed weaker binding properties to PD-1 and VISTA in ELISA (EC50) than the parent antibodies (atezolizumab and onvatilimab). Blockade of VISTA/VSIG-3 binding was also weaker with bsAbs compared to onvatilimab, but the ability to block the PD-1/PD-L1 pathway was slightly better than with atezolizumab. The Fc-based bsAbs showed statistically significant higher levels of lysis of endometrial, breast and pancreatic cancer cells. The symmetric bsAbs (IgG-HC-scFv) showed the most promising therapeutic potential. Higher levels of cancer cell lysis were associated with higher levels of pro-inflammatory cytokines. Both the asymmetric and symmetric bsAbs resulted in higher secretion levels of IFN-γ, TNFα and Granzyme B than anti-VISTA, anti-PD-L1 monotherapy and anti-VISTA/anti-PD-L1 combination therapy.
The high level of tumor cell lysis and increased expression of pro-inflammatory cytokines induced by the Fc-based bsAbs suggest a novel approach for the treatment of pancreatic, endometrial and breast cancer.
Copyright © 2025 Bielski, Barczyński, Mikitiuk, Myrcha, Rykała, Boon, Gąsior, Hec-Gałązka, Holak and Sitar.
Product Citations: 51
In Frontiers in Immunology on 26 May 2025 by Bielski, P., Barczyński, J., et al.
-
Cancer Research
-
Immunology and Microbiology
FLT3L governs the development of partially overlapping hematopoietic lineages in humans and mice.
In Cell on 23 May 2024 by Momenilandi, M., Levy, R., et al.
FMS-related tyrosine kinase 3 ligand (FLT3L), encoded by FLT3LG, is a hematopoietic factor essential for the development of natural killer (NK) cells, B cells, and dendritic cells (DCs) in mice. We describe three humans homozygous for a loss-of-function FLT3LG variant with a history of various recurrent infections, including severe cutaneous warts. The patients' bone marrow (BM) was hypoplastic, with low levels of hematopoietic progenitors, particularly myeloid and B cell precursors. Counts of B cells, monocytes, and DCs were low in the patients' blood, whereas the other blood subsets, including NK cells, were affected only moderately, if at all. The patients had normal counts of Langerhans cells (LCs) and dermal macrophages in the skin but lacked dermal DCs. Thus, FLT3L is required for B cell and DC development in mice and humans. However, unlike its murine counterpart, human FLT3L is required for the development of monocytes but not NK cells.
Copyright © 2024 The Authors. Published by Elsevier Inc. All rights reserved.
-
FC/FACS
-
Homo sapiens (Human)
In IScience on 15 March 2024 by Giovenzana, A., Bezzecchi, E., et al.
Obesity is characterized by the accumulation of T cells in insulin-sensitive tissues, including the visceral adipose tissue (VAT), that can interfere with the insulin signaling pathway eventually leading to insulin resistance (IR) and type 2 diabetes. Here, we found that PD-1+CD4 conventional T (Tconv) cells, endowed with a transcriptomic and functional profile of partially dysfunctional cells, are diminished in VAT of obese patients with dysglycemia (OB-Dys), without a concomitant increase in apoptosis. These cells showed enhanced capacity to recirculate into the bloodstream and had a non-restricted TCRβ repertoire divergent from that of normoglycemic obese and lean individuals. PD-1+CD4 Tconv were reduced in the circulation of OB-Dys, exhibited an altered migration potential, and were detected in the liver of patients with non-alcoholic steatohepatitis. The findings suggest a potential role for partially dysfunctional PD-1+CD4 Tconv cells as inter-organ mediators of IR in obese patients with dysglycemic.
© 2024 The Author(s).
-
Homo sapiens (Human)
-
Cardiovascular biology
-
Immunology and Microbiology
In Nature Communications on 4 January 2024 by Zamora, A., Nougué, M., et al.
Lymphedema (LD) is characterized by the accumulation of interstitial fluid, lipids and inflammatory cell infiltrate in the limb. Here, we find that LD tissues from women who developed LD after breast cancer exhibit an inflamed gene expression profile. Lipidomic analysis reveals decrease in specialized pro-resolving mediators (SPM) generated by the 15-lipoxygenase (15-LO) in LD. In mice, the loss of SPM is associated with an increase in apoptotic regulatory T (Treg) cell number. In addition, the selective depletion of 15-LO in the lymphatic endothelium induces an aggravation of LD that can be rescued by Treg cell adoptive transfer or ALOX15-expressing lentivector injections. Mechanistically, exogenous injections of the pro-resolving cytokine IFN-β restores both 15-LO expression and Treg cell number in a mouse model of LD. These results provide evidence that lymphatic 15-LO may represent a therapeutic target for LD by serving as a mediator of Treg cell populations to resolve inflammation.
© 2024. The Author(s).
-
Immunology and Microbiology
In Clinical Cancer Research on 1 September 2023 by Roschewski, M., Patel, M. R., et al.
Novel targeted and immunotherapies have improved outcomes in relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL), but toxicities limit widespread use. The selective Bruton tyrosine kinase (BTK) inhibitor acalabrutinib has activity in patients with R/R DLBCL but durable responses are uncommon. STAT3 inhibition has demonstrated clinical activity in DLBCL.
Final results of the phase I study of acalabrutinib plus STAT3 inhibitor (danvatirsen; AZD9150) in patients with R/R DLBCL are reported. Danvatirsen 200 mg intravenous infusion [Days 1, 3, 5 (Cycle 1); weekly infusions starting Day 8, Cycle 1] was administered in combination with oral acalabrutinib 100 mg twice daily until progressive disease (PD) or unacceptable toxicity. Primary endpoints were safety and tolerability. Secondary endpoints included efficacy, pharmacokinetics, and immunogenicity.
Seventeen patients received combination treatment. One dose-limiting toxicity (Grade 3 liver transaminase) occurred in 1 patient. The most common reason for treatment discontinuation was PD (65%). In evaluable patients (n = 17), objective response rate was 24%; median duration of response was 1.9 months. All responders with available DLBCL cell-of-origin data were either activated B-cell or nongerminal center B-cell like subtype. Genetic subtype did not correlate with response. Baseline and longitudinal plasma cell-free DNA (cfDNA) concentrations were mostly higher in nonresponding patients. cfDNA changes were generally concordant with imaging. Pretreatment circulating B-cell levels were higher in responders versus nonresponders.
Targeting both STAT3 and BTK in combination is safe and tolerable but efficacy is limited in R/R DLBCL. Results support evaluation of circulating tumor DNA as a biomarker for clinical response.
©2023 The Authors; Published by the American Association for Cancer Research.
-
Homo sapiens (Human)
-
Cancer Research
-
Genetics
-
Immunology and Microbiology
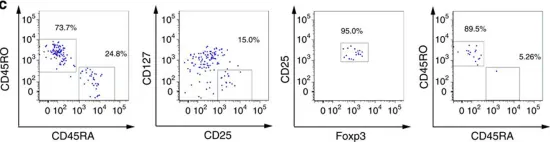
In Nat Commun on 15 March 2016 by Serr, I., Fürst, R. W., et al.
Fig.2.C

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 3
In Front Immunol on 25 February 2015 by Ziegler, H., Welker, C., et al.
Fig.3.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 3
In Front Immunol on 25 February 2015 by Ziegler, H., Welker, C., et al.
Fig.5.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 3