Antagonism of the PD-1/PD-L1 axis is a critical therapeutic strategy for patients with advanced bladder cancer. IFNγ functions as a key regulator of PD-L1 in both immune as well as cancer cells. Forkhead box P3 (FOXP3) is a transcription factor synonymous in T regulatory cell function but with increasingly described functions in cancer cells. Here, we investigated the relationship between FOXP3 and PD-L1 in bladder cancer. We showed that FOXP3 is critical in the ability for IFNγ to activate PD-L1 in bladder cancer cells. FOXP3 can bind to the PD-L1 promoter and induces a gene program that leads to regulation of multiple immune-related genes and genes involved in epithelial-to-mesenchymal transition (EMT). Using in vitro and in vivo human and murine models, we showed that FOXP3 can influence bladder cancer EMT as well as promote cancer metastases. Furthermore, FOXP3 may be a convergent factor for multiple activators of PD-L1, including the chemotherapeutic drug cisplatin.
Historically a key transcription factor driving T regulatory cell function, FOXP3 has an increasingly recognized role in cancer cells. In bladder cancer, we defined a novel mechanism whereby FOXP3 mediates the activation of the immune checkpoint PD-L1 by the cytokine IFNγ. We also showed that FOXP3 induces other immune checkpoints as well as genes involved in EMT, promoting immune resistance and cancer metastases.
©2024 The Authors; Published by the American Association for Cancer Research.
Product Citations: 535
In Cancer Res Commun on 1 August 2024 by Zhang, H., Ly, A., et al.
-
Mus musculus (House mouse)
-
Cancer Research
In Scientific Reports on 3 June 2024 by Wu, S. Y., Wang, C. H., et al.
Pancreatic ductal adenocarcinoma (PDAC) poses challenges due to late-stage diagnosis and limited treatment response, often attributed to the hypoxic tumor microenvironment (TME). Sonoporation, combining ultrasound and microbubbles, holds promise for enhancing therapy. However, additional preclinical research utilizing commercially available ultrasound equipment for PDAC treatment while delving into the TME's intricacies is necessary. This study investigated the potential of using a clinically available ultrasound system and phase 2-proven microbubbles to relieve tumor hypoxia and enhance the efficacy of chemotherapy and immunotherapy in a murine PDAC model. This approach enables early PDAC detection and blood-flow-sensitive Power-Doppler sonoporation in combination with chemotherapy. It significantly extended treated mice's median survival compared to chemotherapy alone. Mechanistically, this combination therapy enhanced tumor perfusion and substantially reduced tumor hypoxia (77% and 67%, 1- and 3-days post-treatment). Additionally, cluster of differentiation 8 (CD8) T-cell infiltration increased four-fold afterward. The combined treatment demonstrated a strengthening of the anti-programmed death-ligand 1(αPDL1) therapy against PDAC. Our study illustrates the feasibility of using a clinically available ultrasound system with NH-002 microbubbles for early tumor detection, alleviating hypoxic TME, and improving chemotherapy and immunotherapy. It suggests the development of an adjuvant theragnostic protocol incorporating Power-Doppler sonoporation for pancreatic tumor treatment.
© 2024. The Author(s).
-
Mus musculus (House mouse)
-
Cancer Research
-
Immunology and Microbiology
In JCI Insight on 12 March 2024 by Jiang, Y., Gruszka, D., et al.
IL-17C is an epithelial cell-derived proinflammatory cytokine whose transcriptional regulation remains unclear. Analysis of the IL17C promoter region identified TCF4 as putative regulator, and siRNA knockdown of TCF4 in human keratinocytes (KCs) increased IL17C. IL-17C stimulation of KCs (along with IL-17A and TNF-α stimulation) decreased TCF4 and increased NFKBIZ and ZC3H12A expression in an IL-17RA/RE-dependent manner, thus creating a feedback loop. ZC3H12A (MCPIP1/Regnase-1), a transcriptional immune-response regulator, also increased following TCF4 siRNA knockdown, and siRNA knockdown of ZC3H12A decreased NFKBIZ, IL1B, IL36G, CCL20, and CXCL1, revealing a proinflammatory role for ZC3H12A. Examination of lesional skin from the KC-Tie2 inflammatory dermatitis mouse model identified decreases in TCF4 protein concomitant with increases in IL-17C and Zc3h12a that reversed following the genetic elimination of Il17c, Il17ra, and Il17re and improvement in the skin phenotype. Conversely, interference with Tcf4 in KC-Tie2 mouse skin increased Il17c and exacerbated the inflammatory skin phenotype. Together, these findings identify a role for TCF4 in the negative regulation of IL-17C, which, alone and with TNF-α and IL-17A, feed back to decrease TCF4 in an IL-17RA/RE-dependent manner. This loop is further amplified by IL-17C-TCF4 autocrine regulation of ZC3H12A and IL-17C regulation of NFKBIZ to promote self-sustaining skin inflammation.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
In Cell Death & Disease on 30 January 2024 by Yang, S. J., Chang, S. T., et al.
Cancer cells can evade immune elimination by activating immunosuppressive signaling pathways in the tumor microenvironment (TME). Targeting immunosuppressive signaling pathways to promote antitumor immunity has become an attractive strategy for cancer therapy. Aurora-A is a well-known oncoprotein that plays a critical role in tumor progression, and its inhibition is considered a promising strategy for treating cancers. However, targeting Aurora-A has not yet got a breakthrough in clinical trials. Recent reports have indicated that inhibition of oncoproteins may reduce antitumor immunity, but the role of tumor-intrinsic Aurora-A in regulating antitumor immunity remains unclear. In this study, we demonstrated that in tumors with high lymphocyte infiltration (hot tumors), higher tumor-intrinsic Aurora-A expression is associated with a better prognosis in CRC patients. Mechanically, tumor-intrinsic Aurora-A promotes the cytotoxic activity of CD8+ T cells in immune hot CRC via negatively regulating interleukin-16 (IL-16), and the upregulation of IL-16 may impair the therapeutic effect of Aurora-A inhibition. Consequently, combination treatment with IL-16 neutralization improves the therapeutic response to Aurora-A inhibitors in immune hot CRC tumors. Our study provides evidence that tumor-intrinsic Aurora-A contributes to anti-tumor immunity depending on the status of lymphocyte infiltration, highlighting the importance of considering this aspect in cancer therapy targeting Aurora-A. Importantly, our results suggest that combining Aurora-A inhibitors with IL-16-neutralizing antibodies may represent a novel and effective approach for cancer therapy, particularly in tumors with high levels of lymphocyte infiltration.
© 2024. The Author(s).
-
FC/FACS
-
Mus musculus (House mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
In Aging (Albany NY) on 14 July 2023 by Su, B., Li, R., et al.
Asthma is a chronic inflammatory disease with a high morbidity rate in children and significantly impacts their healthy growth. It is reported that Th2 cell-mediated airway inflammation and activated oxidative stress are involved in the pathogenesis of asthma. S14G-humanin (HNG) is a derivative of Humanin with higher activity. The present study proposes to explore the potential treating property of HNG on asthma. An asthma model was constructed in mice using ovalbumin (OVA), the mice were treated with 2.5 mg/kg and 5 mg/kg HNG for 16 days. Dramatically increased lung weight index, elevated number of monocytes, eosinophils, and neutrophils, promoted production of Th2 cytokines including interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-13 (IL-13), and severe histological pathology were observed in OVA-challenged mice, all of which were extremely alleviated by 2.5 mg/kg and 5 mg/kg HNG. Furthermore, the increased malondialdehyde (MDA) level and declined superoxide dismutase (SOD) activity in OVA-challenged mice were abolished by 2.5 mg/kg and 5 mg/kg HNG. Lastly, the upregulated TLR4, p-NF-κB p65, and early growth response 1 (Egr-1) in lung tissues of OVA-challenged mice were pronouncedly downregulated by 2.5 mg/kg and 5 mg/kg HNG. Collectively, our data suggested that HNG ameliorated airway inflammation in asthma partially due to NF-κB and Egr-1-mediated responses.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
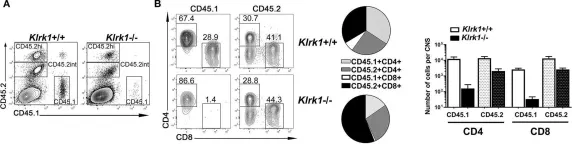
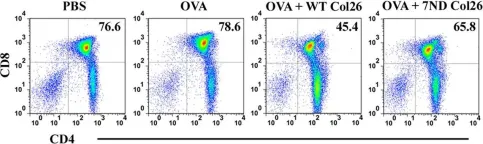
In Front Immunol on 23 February 2019 by Legroux, L., Moratalla, A. C., et al.
Fig.7.A

-
FC/FACS
-
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 15
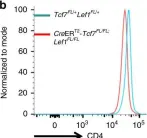
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.2.D

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
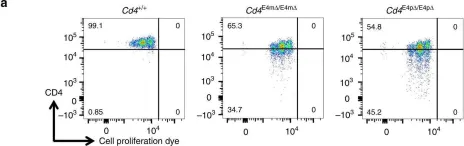
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.2.A

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
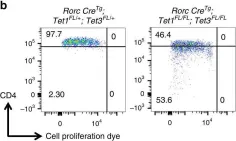
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.3.A

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.4.B

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.4.C

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.4.E

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.5.A

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.6.A

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.6.B

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 5 September 2018 by Issuree, P. D., Day, K., et al.
Fig.1.D

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In Nat Commun on 26 September 2017 by Kojo, S., Tanaka, H., et al.
Fig.6.D

-
FC/FACS
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 15
In PLoS One on 21 July 2012 by Baba, T., Badr, M. e. l. S., et al.
Fig.4.F

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 15
In J Neuroinflammation on 16 January 2012 by Lee, E., Chanamara, S., et al.
Fig.4.A

-
IHC-IF
-
Mus musculus (House mouse)
Collected and cropped from J Neuroinflammation by CiteAb, provided under a CC-BY license
Image 1 of 15
In PLoS Pathog on 1 October 2009 by Bai, F., Town, T., et al.
Fig.8.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from PLoS Pathog by CiteAb, provided under a CC-BY license
Image 1 of 15