Standard treatment for newly diagnosed high-grade gliomas remains suboptimal. Preclinical data indicate that mesenchymal transition and radiation resistance in glioblastoma are driven by NF-κB and microglia activation, which can be inhibited by minocycline. We assessed the safety and efficacy of minocycline combined with standard radiation and temozolomide in newly diagnosed high-grade gliomas.
Adults with newly diagnosed high-grade glioma were eligible. Minocycline was given with concurrent and adjuvant temozolomide. Minocycline doses were escalated using a 3 + 3 design and expanded to identify the maximum tolerated dose (MTD) and adverse event profile. Individual progression-free survival (PFS) was compared to predicted PFS based on RTOG RPA class using a binomial test. The relationships between mesenchymal and microglial biomarkers were analyzed with immunohistochemistry.
The MTD of minocycline was 150 mg twice per day (N = 20); 1 patient (5%) experienced CTCAE grade 3 + nausea and dizziness, and 2 patients (10%) demonstrated thrombocytopenia requiring temozolomide interruptions. Twelve patients exceeded their predicted PFS (60%), which did not meet the predefined efficacy endpoint of 70%. Symptoms increased during post-radiation treatment but remained mild. No significant correlation was seen between biomarkers and PFS. Expression levels of P-p65, a marker of NF-κB activation, were correlated with the microglia marker IBA-1.
Minocycline at 150 mg twice per day is well tolerated with standard chemoradiation in patients with newly diagnosed high-grade gliomas. PFS was not significantly increased with the addition of minocycline when compared to historical controls. NF-κB activation correlates with microglia levels in high-grade glioma.
© The Author(s) 2024. Published by Oxford University Press, the Society for Neuro-Oncology and the European Association of Neuro-Oncology.
Product Citations: 57
In Neuro-oncology Advances on 27 May 2024 by McKean, W. B., Yang, J., et al.
-
Homo sapiens (Human)
-
Cancer Research
In Frontiers in Oncology on 29 November 2023 by Padevit, L., Vasella, F., et al.
The selection of patients for further therapy after meningioma surgery remains a challenge. Progress has been made in this setting in selecting patients that are more likely to have an aggressive disease course by using molecular tests such as gene panel sequencing and DNA methylation profiling. The aim of this study was to create a preselection tool warranting further molecular work-up.
All patients undergoing surgery for resection or biopsy of a cranial meningioma from January 2013 until December 2018 at the University Hospital Zurich with available tumor histology were included. Various prospectively collected clinical, radiological, histological and immunohistochemical variables were analyzed and used to train a logistic regression model to predict tumor recurrence or progression. Regression coefficients were used to generate a scoring system grading every patient into low, intermediate, and high-risk group for tumor progression or recurrence.
Out of a total of 13 variables preselected for this study, previous meningioma surgery, Simpson grade, progesterone receptor staining as well as presence of necrosis and patternless growth on histopathological analysis of 378 patients were included into the final model. Discrimination showed an AUC of 0.81 (95% CI 0.73 - 0.88), the model was well-calibrated. Recurrence-free survival was significantly decreased in patients in intermediate and high-risk score groups (p-value < 0.001).
The proposed prediction model showed good discrimination and calibration. This prediction model is based on easily obtainable information and can be used as an adjunct for patient selection for further molecular work-up in a tertiary hospital setting.
Copyright © 2023 Padevit, Vasella, Friedman, Mutschler, Jenkins, Held, Rushing, Wirsching, Weller, Regli and Neidert.
-
IHC
-
Homo sapiens (Human)
-
Cancer Research
In Frontiers in Cell and Developmental Biology on 30 August 2023 by Rojas, F., Aguilar, R., et al.
Astrocytes play a critical role in the maintenance of a healthy central nervous system and astrocyte dysfunction has been implicated in various neurodegenerative disorders, including amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD). There is compelling evidence that mouse and human ALS and ALS/FTD astrocytes can reduce the number of healthy wild-type motoneurons (MNs) in co-cultures or after treatment with astrocyte conditioned media (ACM), independently of their genotype. A growing number of studies have shown that soluble toxic factor(s) in the ACM cause non-cell autonomous MN death, including our recent identification of inorganic polyphosphate (polyP) that is excessively released from mouse primary astrocytes (SOD1, TARDBP, and C9ORF72) and human induced pluripotent stem cells (iPSC)-derived astrocytes (TARDBP) to kill MNs. However, others have reported that astrocytes carrying mutant TDP43 do not produce detectable MN toxicity. This controversy is likely to arise from the findings that human iPSC-derived astrocytes exhibit a rather immature and/or reactive phenotype in a number of studies. Here, we have succeeded in generating a highly homogenous population of functional quiescent mature astrocytes from control subject iPSCs. Using identical conditions, we also generated mature astrocytes from an ALS/FTD patient carrying the TDP43A90V mutation. These mutant TDP43 patient-derived astrocytes exhibit key pathological hallmarks, including enhanced cytoplasmic TDP-43 and polyP levels. Additionally, mutant TDP43 astrocytes displayed a mild reactive signature and an aberrant function as they were unable to promote synaptogenesis of hippocampal neurons. The polyP-dependent neurotoxic nature of the TDP43A90V mutation was further confirmed as neutralization of polyP in ACM derived from mutant TDP43 astrocytes prevented MN death. Our results establish that human astrocytes carrying the TDP43A90V mutation exhibit a cell-autonomous pathological signature, hence providing an experimental model to decipher the molecular mechanisms underlying the generation of the neurotoxic phenotype.
Copyright © 2023 Rojas, Aguilar, Almeida, Fritz, Corvalán, Ampuero, Abarzúa, Garcés, Amaro, Diaz, Arredondo, Cortes, Sanchez, Mercado, Varela-Nallar, Gao, Montecino and van Zundert.
-
Neuroscience
-
Stem Cells and Developmental Biology
Tissue factor is a critical regulator of radiation therapy-induced glioblastoma remodeling.
In Cancer Cell on 14 August 2023 by Jeon, H. M., Kim, J. Y., et al.
Radiation therapy (RT) provides therapeutic benefits for patients with glioblastoma (GBM), but inevitably induces poorly understood global changes in GBM and its microenvironment (TME) that promote radio-resistance and recurrence. Through a cell surface marker screen, we identified that CD142 (tissue factor or F3) is robustly induced in the senescence-associated β-galactosidase (SA-βGal)-positive GBM cells after irradiation. F3 promotes clonal expansion of irradiated SA-βGal+ GBM cells and orchestrates oncogenic TME remodeling by activating both tumor-autonomous signaling and extrinsic coagulation pathways. Intratumoral F3 signaling induces a mesenchymal-like cell state transition and elevated chemokine secretion. Simultaneously, F3-mediated focal hypercoagulation states lead to activation of tumor-associated macrophages (TAMs) and extracellular matrix (ECM) remodeling. A newly developed F3-targeting agent potently inhibits the aforementioned oncogenic events and impedes tumor relapse in vivo. These findings support F3 as a critical regulator for therapeutic resistance and oncogenic senescence in GBM, opening potential therapeutic avenues.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Cancer Research
In Cell Death & Disease on 8 August 2023 by Steffens Reinhardt, L., Groen, K., et al.
In breast cancer, dysregulated TP53 expression signatures are a better predictor of chemotherapy response and survival outcomes than TP53 mutations. Our previous studies have shown that high levels of Δ40p53 are associated with worse disease-free survival and disruption of p53-induced DNA damage response in breast cancers. Here, we further investigated the in vitro and in vivo implications of Δ40p53 expression in breast cancer. We have shown that genes associated with cell differentiation are downregulated while those associated with stem cell regulation are upregulated in invasive ductal carcinomas expressing high levels of Δ40p53. In contrast to p53, endogenous ∆40p53 co-localised with the stem cell markers Sox2, Oct4, and Nanog in MCF-7 and ZR75-1 cell lines. ∆40p53 and Sox2 co-localisation was also detected in breast cancer specimens. Further, in cells expressing a high ∆40p53:p53 ratio, increased expression of stem cell markers, greater mammosphere and colony formation capacities, and downregulation of miR-145 and miR-200 (p53-target microRNAs that repress stemness) were observed compared to the control subline. In vivo, a high ∆40p53:p53 ratio led to increased tumour growth, Ki67 and Sox2 expression, and blood microvessel areas in the vehicle-treated mice. High expression of ∆40p53 also reduced tumour sensitivity to doxorubicin compared to control tumours. Enhanced therapeutic efficacy of doxorubicin was observed when transiently targeting Δ40p53 or when treating cells with OTSSP167 with concomitant chemotherapy. Taken together, high Δ40p53 levels induce tumour growth and may promote chemoresistance by inducing a stemness phenotype in breast cancer; thus, targeting Δ40p53 in tumours that have a high Δ40p53:p53 ratio could enhance the efficacy of standard-of-care therapies such as doxorubicin.
© 2023. The Author(s).
-
WB
-
FC/FACS
-
Homo sapiens (Human)
-
Cancer Research
-
Cell Biology
In Sci Adv on 15 April 2022 by Mastrogiovanni, M., Vargas, P., et al.
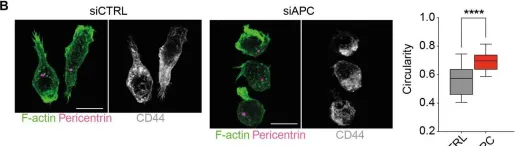
Fig.5.B

-
ICC-IF
-
Homo sapiens (Human)
Collected and cropped from Sci Adv by CiteAb, provided under a CC-BY license
Image 1 of 5
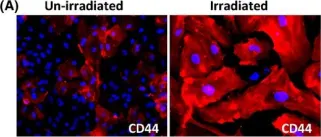
In Aging Cell on 1 October 2014 by Lowe, D. & Raj, K.
Fig.4.A

-
IF
-
Homo sapiens (Human)
Collected and cropped from Aging Cell by CiteAb, provided under a CC-BY license
Image 1 of 5
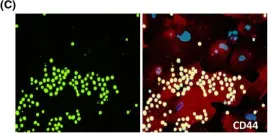
In Aging Cell on 1 October 2014 by Lowe, D. & Raj, K.
Fig.4.C

-
IF
-
Homo sapiens (Human)
Collected and cropped from Aging Cell by CiteAb, provided under a CC-BY license
Image 1 of 5
In PLoS One on 3 May 2013 by Gammon, L., Biddle, A., et al.
Fig.2.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 5
In BMC Cancer on 29 September 2010 by Eberth, S., Schneider, B., et al.
Fig.6.A

-
FC/FACS
-
Collected and cropped from BMC Cancer by CiteAb, provided under a CC-BY license
Image 1 of 5