As pyrazole and its derivatives have a wide range of biological activities, including anticancer activity, the design of novel pyrazole derivatives has emerged as an important research field. This study describes a novel pyrazole derivative that exerts antitumor and radiosensitizing activities in breast cancer both in vitro and in vivo. We synthesized a novel pyrazole compound N,N-dimethyl-N'-(3-(1-(4-(trifluoromethyl)phenyl)-1H-pyrazol-4-yl)phenyl)azanesulfonamide (PCW-1001) and showed that it inhibited several oncogenic properties of breast cancer both in vitro and in vivo. PCW-1001 induced apoptosis in several breast cancer cell lines. Transcriptome analysis of PCW-1001-treated cells showed that it regulates genes involved in the DNA damage response, suggesting its potential use in radiotherapy. Indeed, PCW-1001 enhanced the radiation sensitivity of breast cancer cells by modulating the expression of DNA damage response genes. Therefore, our data describe a novel pyrazole compound, PCW-1001, with antitumor and radiosensitizer activities in breast cancer.
Copyright © 2022 Kang, Pandit, Kim, Cho, Kwon, Ahn, Lee, Wu, Oh, Jung and Kim.
Product Citations: 9
In Frontiers in Oncology on 16 April 2022 by Kang, M., Pandit, N., et al.
-
WB
-
Homo sapiens (Human)
-
Cancer Research
HDAC6-Selective Inhibitor Overcomes Bortezomib Resistance in Multiple Myeloma.
In International Journal of Molecular Sciences on 29 January 2021 by Lee, S. W., Yeon, S. K., et al.
Although multiple myeloma (MM) patients benefit from standard bortezomib (BTZ) chemotherapy, they develop drug resistance, resulting in relapse. We investigated whether histone deacetylase 6 (HDAC6) inhibitor A452 overcomes bortezomib resistance in MM. We show that HDAC6-selective inhibitor A452 significantly decreases the activation of BTZ-resistant markers, such as extracellular signal-regulated kinases (ERK) and nuclear factor kappa B (NF-κB), in acquired BTZ-resistant MM cells. Combination treatment of A452 and BTZ or carfilzomib (CFZ) synergistically reduces BTZ-resistant markers. Additionally, A452 synergizes with BTZ or CFZ to inhibit the activation of NF-κB and signal transducer and activator of transcription 3 (STAT3), resulting in decreased expressions of low-molecular-mass polypeptide 2 (LMP2) and LMP7. Furthermore, combining A452 with BTZ or CFZ leads to synergistic cancer cell growth inhibition, viability decreases, and apoptosis induction in the BTZ-resistant MM cells. Overall, the synergistic effect of A452 with CFZ is more potent than that of A452 with BTZ in BTZ-resistant U266 cells. Thus, our findings reveal the HDAC6-selective inhibitor as a promising therapy for BTZ-chemoresistant MM.
-
Homo sapiens (Human)
In Chemotherapy on 30 October 2018 by Khoury, H., He, R., et al.
Acute myeloid leukemia (AML) continues to be a deadly disease, with only 50-70% of patients achieving complete remission and less than 30% of adults having sustained long-term remissions. In order to address these unmet medical needs, we carried out a high-throughput screen of an in-house library of on- and off-patent drugs with the OCI/AML-2 cell line. Through this screen, we discovered adefovir dipi-voxil (adefovir-DP) as being active against human AML. In addition to adefovir-DP, there are second-generation formulations of adefovir, including octadecyloxyethyl adefovir (ODE-adefovir) and hexadecyloxypropyl adefovir (HDP-adefovir), which were designed to overcome the pharmacokinetic problems of the parent compound adefovir. Given the known clinical benefit of nucleoside analogs for the treatment of AML, we undertook studies to evaluate the potential benefit of adefovir-based molecules. In AML cell lines and patient samples, adefovir-DP and ODE-adefovir were highly potent, whereas HDP-adefovir was significantly less active. Interestingly, ODE-adefovir was remarkably less toxic than adefovir-DP towards normal hematopoietic cells. In addition, ODE-adefovir at a dose of 15 mg/kg/day showed potent activity against human AML in a NOD/SCID mouse model, with a reduction of human leukemia in mouse bone marrow of > 40% in all mice tested within 20 days of treatment. Based on its chemical structure, we hypothesized that the cytotoxicity of ODE-adefovir toward AML was through cell cycle arrest and DNA damage. Indeed, ODE-adefovir treatment induced cell cycle arrest in the S phase and increased levels of pH2Ax, indicating the induction of DNA damage. Furthermore, there was an increase in phospho-p53, transactivation of proapoptotic genes and activation of the intrinsic apoptotic pathway. Subsequent investigation unveiled strong synergism between ODE-adefovir and ara-C, making their coadministration of potential clinical benefit. Expression of MRP4, a nucleoside transporter, appeared to influence the response of AML cells to ODE-adefovir, as its inhibition potentiated ODE-adefovir killing. Taken together, our findings indicate that clinical development of ODE-adefovir or related compounds for the treatment of AML is warranted.
© 2018 S. Karger AG, Basel.
-
WB
-
Cancer Research
In Journal of Korean Medical Science on 1 September 2014 by Kim, S. G., Ahn, S. Y., et al.
The expression of hypoxia-inducible factor (HIF) is influenced by reactive oxygen species (ROS). Effect of bilirubin on HIF-1 expression in proximal tubular cells was investigated under physiological oxygen concentration, which is relative hypoxic condition mimicking oxygen content in the medulla of renal tissue. The human kidney (HK2) cells were cultured in 5% oxygen with or without bilirubin. HIF-1α protein expression was increased by bilirubin treatment at 0.01-0.2 mg/dL concentration. The messenger RNA expression of HIF-1α was increased by 1.69±0.05 folds in the cells cultured with 0.1 mg/dL bilirubin, compared to the control cells. The inhibitors of PI3K/mTOR, PI3K/AKT, and ERK 1/2 pathways did not attenuate increased HIF-1α expression by bilirubin. HIF-1α expression decreased by 10 µM exogenous hydrogen peroxide (H2O2); scavenger of ROS with or without bilirubin in the HK2 cells increased HIF-1α concentration more than that in the cells without bilirubin. Exogenous H2O2 decreased the phosphorylation of P70S6 kinase, which was completely reversed by bilirubin treatment. Knockdown of NOX4 gene by small interfering RNA (siRNA) increased HIF-1α mRNA expression. In coonclusion, bilirubin enhances HIF-1α transcription as well as the up-regulation of HIF-1α protein translation through the attenuation of ROS and subunits of NADPH oxidase.
-
WB
-
Biochemistry and Molecular biology
In Nucleic Acids Research on 1 October 2010 by Lin, S. Y., Hsueh, C. M., et al.
Carcinogenesis is determined based on both cell proliferation and death rates. Recent studies demonstrate that heat shock proteins (HSPs) regulate apoptosis. HLJ1, a member of the DnaJ-like Hsp40 family, is a newly identified tumor suppressor protein closely related to relapse and survival in non-small cell lung cancer (NSCLC) patients. However, its role in apoptosis is currently unknown. In this study, NSCLC cell lines displaying varying HLJ1 expression levels were subjected to ultraviolet (UV) irradiation, followed by flow cytometry. Interestingly, the percentages of apoptotic cells in the seven cell lines examined were positively correlated with HLJ1 expression. Enforcing expression of HLJ1 in low-HLJ1 expressing highly invasive cells promoted UV-induced apoptosis through enhancing JNK and caspase-3 activation in NSCLC. Additionally, UV irradiation led to reduced levels of HLJ1 predominantly in apoptotic cells. The pan-caspase inhibitor, zVAD-fmk and caspase-3-specific inhibitor, DEVD-fmk, prevented UV-induced degradation of HLJ1 by the late stage of apoptosis. Further experiments revealed a non-typical caspase-3 cleavage site (MEID) at amino acid 125-128 of HLJ1. Our results collectively suggest that HLJ1 is a novel substrate of caspase-3 during the UV-induced apoptotic process.
-
WB
-
Biochemistry and Molecular biology
-
Cancer Research
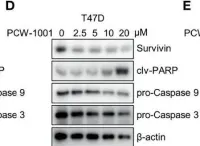
In Front Oncol on 16 April 2022 by Kang, M., Pandit, N., et al.
Fig.4.D

-
WB
-
Homo sapiens (Human)
Collected and cropped from Front Oncol by CiteAb, provided under a CC-BY license
Image 1 of 3
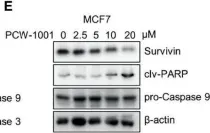
In Front Oncol on 16 April 2022 by Kang, M., Pandit, N., et al.
Fig.4.E

-
WB
-
Homo sapiens (Human)
Collected and cropped from Front Oncol by CiteAb, provided under a CC-BY license
Image 1 of 3
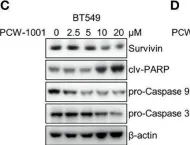
In Front Oncol on 16 April 2022 by Kang, M., Pandit, N., et al.
Fig.4.C

-
WB
-
Homo sapiens (Human)
Collected and cropped from Front Oncol by CiteAb, provided under a CC-BY license
Image 1 of 3