Adipose-derived mesenchymal stem cells (AD-MSCs) have emerged as a promising source for cardiac regenerative therapy due to their multipotency and ease of isolation. However, the impact of anatomical origin on their cardiomyocyte differentiation potential remains unclear. Metabolic analysis provides valuable real-time insights into the cellular metabolic state, capturing dynamic changes in metabolite concentrations that reflect both internal cellular mechanisms and external stimuli. This approach allows us to identify specific metabolic pathways activated during cardiomyocyte differentiation, offering a deeper understanding of how the anatomical origin of stem cells influences their differentiation potential and metabolic flexibility. Such insights are critical for optimizing stem cell-based therapies for cardiac regeneration. This study aimed to compare the differentiation capacity of AD-MSCs derived from peri-ovarian and peri-renal adipose tissue, with a focus on metabolic adaptations during cardiomyocyte differentiation.
AD-MSCs were isolated from peri-ovarian and peri-renal fat of Sprague-Dawley rats and characterized by morphology, immunophenotyping, and multilineage differentiation potential. Cardiomyocyte differentiation was induced using 5-azacytidine, and morphological changes were assessed via phase-contrast microscopy and immunofluorescence staining for cardiac troponin T (cTnT). Untargeted metabolomic profiling was performed using gas chromatography-mass spectrometry (GC-MS), followed by principal component analysis (PCA), partial least squares discriminant analysis (PLS-DA), and pathway enrichment analysis.
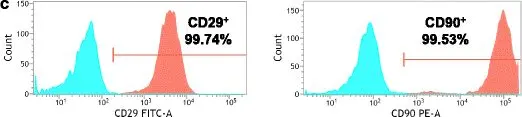
Both peri-ovarian and peri-renal AD-MSCs exhibited similar fibroblast-like morphology, MSC-specific marker expression (CD44, CD90, CD29), and multilineage differentiation potential. Following cardiomyocyte induction, both groups displayed morphological changes indicative of differentiation and strong cTnT expression. Metabolomic analysis of the cardiogenic differentiation samples identified distinct metabolic adaptations between the two AD-MSC sources. Peri-ovarian AD-MSCs exhibited a broader metabolic reprogramming, with increased engagement of glycolysis, fructose metabolism, glycerolipid metabolism, and the TCA cycle, suggesting enhanced metabolic flexibility and energy efficiency. In contrast, peri-renal AD-MSCs relied more on galactose metabolism, indicating an alternative energy strategy during differentiation.
The anatomical origin of AD-MSCs influences their metabolic landscape during cardiomyocyte differentiation. Peri-ovarian AD-MSCs demonstrated greater metabolic adaptability, potentially favoring their differentiation capacity, making them a promising candidate for cardiac regenerative applications.
Copyright © 2025 Farag, Samir, Koung Ngeun, Kaneda, Hendawy, Takahashi and Tanaka.
Product Citations: 69
In Frontiers in Cell and Developmental Biology on 4 July 2025 by Farag, A., Samir, H., et al.
-
FC/FACS
-
Rattus norvegicus (Rat)
-
Stem Cells and Developmental Biology
In BMC Oral Health on 18 September 2024 by El Qashty, R. M. N., Youssef, J. M., et al.
Tongue defects have several etiologies and significantly affect the quality of life. This study was conducted to compare the regenerative potential of erythropoietin (EPO)-loaded hydrogel and adipose derived stem cell (ADSC) secretome on tongue dorsum defects focusing on the role of anti-inflammatory M2 macrophage phenotype.
Rats were subjected to induction of mechanical circular defects on the dorsal surface of the tongue, then divided into three groups; Group I (control): received 0.1 ml phosphate buffered saline, Group II (EPO): received 5000 U/kg EPO-hydrogel, and Group III (ADSC-Secretome): received 0.1 ml ADSC-Secretome. Treatments were injected circumferentially around wound margins after induction. Seven and fourteen days after treatment, specimens were obtained and processed for histological and immunohistochemical staining followed by the relevant histomorphometric and statistical analyses.
Seven days after treatment, groups II and III presented defects with some epithelial regeneration at the lateral margins, while the center of the defect showed granulation tissue with much inflammatory cells. The base of the defects showed some muscle fibers and new blood vessels, however group III showed more enhanced neovascularization. Fourteen days after therapeutic intervention, group II defects were completely covered with epithelium showing a thin keratin layer with regular rete pegs interdigitating with the underlying connective tissue papillae, but tongue papillae were not restored. Group III expressed much better healing with developing filiform papillae. The connective tissue showed more vascularity and well-arranged muscle bundles. Both treated groups showed a significant decrease in defect depth and significant increase in anti-inflammatory macrophages compared to the control group at both time intervals, however there was no significant difference between the two treated groups.
Both treatments showed promising and comparable results in the treatment of tongue defects reducing inflammation and restoring tongue histological architecture with significant upregulation of M2 macrophage.
© 2024. The Author(s).
-
Rattus norvegicus (Rat)
-
Endocrinology and Physiology
-
Stem Cells and Developmental Biology
In BMC Oral Health on 5 October 2023 by El Qashty, R. M. N., Elkashty, O. A., et al.
Temporomandibular joint (TMJ) arthritis is a debilitating, challenging condition and different methods have been implicated for its treatment. This study aimed to test the therapeutic potentials of low-level laser therapy (LLLT) associated with adipose derived stem cells (ADSC) or their derived secretome on a murine model induced arthritis.
Forty eight rats were divided into four groups where group I was the sham control, the rest of animals were subjected to arthritis induction using complete Freund's adjuvant, then divided as follows: group II received phosphate buffered saline (PBS) intraarticular injection and irradiation of 0 j/cm2, group III received ADSCs derived secretome and irradiation of 38 j/cm2, and group IV received ADSCs and irradiation of 38 j/cm2 as well. One and three weeks after treatment, animals were euthanized, and paraffin blocks were processed for histological assessment by hematoxylin and eosin stain with histomorphometrical analysis. Histochemical evaluation of joint proteoglycan content was performed through toluidine blue stain, and immunohistochemical staining by the proinflammatory marker tumor necrosis factor-α (TNF-α) was performed followed by the relevant statistical tests.
The arthritis group showed histological signs of joint injury including cartilage atrophy, articular disc fibrosis, irregular osteochondral interface, and condylar bone resorption together with high inflammatory reaction and defective proteoglycan content. In contrast, the treated groups III and IV showed much restoration of the joint structure with normal cartilage and disc thickness. The inflammation process was significantly suppressed especially after three weeks as confirmed by the significant reduction in TNF-α positive immunostaining compared to the arthritic group, and the cartilage proteoglycan content also showed significant increase relative to the arthritic group. However, no significant difference between the results of the two treated groups was detected.
LLLT conjugated with ADSCs or ADSCs derived secretome can efficiently enhance the healing of arthritic TMJs. Stem cell secretome can be applied as a safe, potent therapy. However, further investigations are required to unravel its mechanism of action and pave its way as a safe, novel, cell free therapy.
© 2023. BioMed Central Ltd., part of Springer Nature.
-
FC/FACS
-
Rattus norvegicus (Rat)
-
Stem Cells and Developmental Biology
In Stem Cell Research & Therapy on 20 March 2023 by Xu, Y. N., Xu, W., et al.
Cholestatic liver fibrosis (CLF) is caused by inflammatory destruction of the intrahepatic bile duct and abnormal proliferation of the small bile duct after cholestasis. Activation of the Notch signaling pathway is required for hepatic stem cells to differentiate into cholangiocytes during the pathogenesis of CLF. Our previous research found that the expression of the Numb protein, a negative regulator of Notch signaling, was significantly reduced in the livers of patients with primary biliary cholangitis and CLF rats. However, the relationship between the Numb gene and CLF is largely unclear. In this study, we investigated the role of the Numb gene in the treatment of bile duct ligation (BDL)-induced CLF.
In vivo, bone marrow-derived mesenchymal stem cells (BM-MSCs) with Numb gene overexpression or knockdown obtained using lentivirus transfection were transplanted into the livers of rats with BDL-induced CLF. The effects of the Numb gene on stem cell differentiation and CLF were evaluated by performing histology, tests of liver function, and measurements of liver hydroxyproline, cytokine gene and protein levels. In vitro, the Numb gene was overexpressed or knocked down in the WB-F344 cell line by lentivirus transfection, Then, cells were subjected immunofluorescence staining and the detection of mRNA levels of related factors, which provided further evidence supporting the results from in vivo experiments.
BM-MSCs overexpressing the Numb gene differentiated into hepatocytes, thereby inhibiting CLF progression. Conversely, BM-MSCs with Numb knockdown differentiated into biliary epithelial cells (BECs), thereby promoting the ductular reaction (DR) and the progression of CLF. In addition, we confirmed that knockdown of Numb in sodium butyrate-treated WB-F344 cells aggravated WB-F344 cell differentiation into BECs, while overexpression of Numb inhibited this process.
The transplantation of BM-MSCs overexpressing Numb may be a useful new treatment strategy for CLF.
© 2023. The Author(s).
-
Stem Cells and Developmental Biology
In Cell Proliferation on 1 February 2023 by Wei, X., Ma, W., et al.
Spina bifida aperta (SBA) is one of the most common neural tube defects. Neural injury in SBA occurs in two stages involving failed neural tube closure and progressive degeneration through contact with the amniotic fluid. We previously suggested that intra-amniotic bone marrow-derived mesenchymal stem cell (BMSC) therapy for fetal rat SBA could achieve beneficial functional recovery through lesion-specific differentiation. The aim of this study is to examine whether the amniotic fluid microenvironment can be improved by intra-amniotic BMSC transplantation.
The intra-amniotic BMSC injection was performed using in vivo rat fetal SBA models. The various cytokine expressions in rat amniotic fluid were screened by protein microassays. Intervention experiments were used to study the function of differentially expressed cytokines.
A total of 32 cytokines showed significant upregulated expression in the BMSC-injected amniotic fluid. We focused on Activin A, NGF, BDNF, CNTF, and CXCR4. Intervention experiments showed that the upregulated Activin A, NGF, BDNF, and CNTF could inhibit apoptosis and promote synaptic development in fetal spinal cords. Inhibiting the activity of these factors weakened the anti-apoptotic and pro-differentiation effects of transplanted BMSCs. Inhibition of CXCR4 activity reduced the engraftment rate of BMSCs in SBA fetuses.
BMSC transplantation can improve the amniotic fluid environment, and this is beneficial for SBA repair.
© 2022 The Authors. Cell Proliferation published by Beijing Institute for Stem Cell and Regenerative Medicine and John Wiley & Sons Ltd.
-
FC/FACS
-
Rattus norvegicus (Rat)
-
Stem Cells and Developmental Biology
In Stem Cell Res Ther on 21 November 2017 by Yang, H., Wu, S., et al.
Fig.1.C

-
FC/FACS
-
Rattus norvegicus (Rat)
Collected and cropped from Stem Cell Res Ther by CiteAb, provided under a CC-BY license
Image 1 of 1