Mutations that negatively impact mitochondrial function are highly prevalent in humans and lead to disorders with a wide spectrum of disease phenotypes, including deficiencies in immune cell development and/or function. Previous analyses of mice with a hepatocyte-specific cytochrome c oxidase (COX) deficiency revealed an unexpected peripheral blood leukopenia associated with splenic and thymic atrophy. Here, we use mice with a hepatocyte-specific deletion of the COX assembly factor Sco1 to show that metabolic defects extrinsic to the hematopoietic compartment lead to a pan-lymphopenia represented by severe losses in both B and T cells. We further demonstrate that immune defects in these mice are associated with the loss of bone marrow lymphoid progenitors common to both lineages and early signs of autoantibody-mediated autoimmunity. Our findings collectively identify hepatocyte dysfunction as a potential instigator of immunodeficiency in patients with congenital mitochondrial defects who suffer from chronic or recurrent infections.
© 2025 The Author(s).
Product Citations: 45
In IScience on 18 April 2025 by Pioli, K. T., Ghosh, S., et al.
In STAR Protocols on 20 September 2024 by Shanmugavadivu, A., Carter, K., et al.
The intestinal lamina propria (LP) is a leukocyte-rich cornerstone of the immune system owing to its vital role in immune surveillance and barrier defense against external pathogens. Here, we present a protocol for isolating and analyzing immune cell subsets from the mouse intestinal LP for further downstream applications. Starting from tissue collection and cleaning, epithelium removal, and enzymatic digestion to collection of single cells, we explain each step in detail to maximize the yield of immune cells from the intestinal LP.
Copyright © 2024 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Immunology and Microbiology
Protocol to Isolate Germinal Centers by Laser Microdissection.
In Bio-protocol on 5 June 2022 by Bahreini, F., Niebuhr, M., et al.
During adaptive immune responses, germinal centers (GC) appear as transient microstructures, in which antigen-specific B and T cells interact with each other. Because only the antigen-activated B and T cells, such as Plasmablasts or follicular T helper (Tfh) cells, are present in GC, the in depth-analysis of GC is of great interest. To identify the cells that reside within GC, the majority of studies use the expression of specific surface molecules for analysis by flow cytometry. To do so, the tissue has to be disrupted for the preparation of single-cell suspensions. Thereby, the local information regarding neighborhoods of B cells and T cells and their potential interaction is lost. To study GC in vivo within their original microenvironment, we established a protocol for the isolation of GC by laser microdissection. To enable the identification of GC for subsequent transcriptomic analysis, the degradation of mRNA was diminished by using frozen tissues and by establishing a rapid staining protocol. This procedure enables histological and transcriptomic analysis of individual GC even within one lymphoid organ.
Copyright © The Authors; exclusive licensee Bio-protocol LLC.
In Bio-protocol on 20 May 2022 by Bahreini, F., Niebuhr, M., et al.
Autoreactive T cells in autoantibody-mediated autoimmune diseases can be divided into two major subsets: (i) follicular T helper cells (Tfh) that provide T cell help in germinal centers (GC) and (ii) effector T (Teff) cells that immigrate into peripheral tissue sites such as the skin and mediate local inflammation. To study the sequence of events leading to the loss of tolerance in autoantibody-mediated autoimmune diseases it is required to investigate both T cell subsets simultaneously. This approach is hampered mainly because the appearance of skin inflammation in mouse models is a random process, which makes it difficult to define the location of inflammation at the right time point. To overcome this problem, we developed a scratching technique for ear skins that leads to the establishment of chronic autoimmune wounds in the mouse model for the pemphigoid-like disease epidermolysis bullosa acquisita. By defining the exact place where the skin wounds should form, this protocol enables a detailed analysis of skin-immigrating Teff cells. Of note, this protocol induces GC in draining lymph nodes in parallel so that Tfh cells in GC can be investigated concurrently. This protocol is not restricted to T cells and can be used for any other skin-immigrating inflammatory cells.
Copyright © The Authors; exclusive licensee Bio-protocol LLC.
ADAM12 is a costimulatory molecule that determines Th1 cell fate and mediates tissue inflammation.
In Cellular Molecular Immunology on 1 August 2021 by Liu, Y., Bockermann, R., et al.
A disintegrin and metalloproteinase (ADAM)12 was previously found to be expressed in T cells in the inflamed brain. However, the function of ADAM12 in T-cell responses in general and in tissue inflammation has not been examined. Here, we studied the role of ADAM12 in T-cell responses, fate determination on activation, and its functions in T cells to mediate tissue inflammation. We identified ADAM12 as a costimulatory molecule that is expressed on naive T cells and downregulated on stimulation. ADAM12 mimics CD28 costimulatory signaling to activate and induce the proliferation of T-helper 1 (Th1) cells. Monoclonal ADAM12 Fab antibodies trigger T-cell activation by amplifying TCR signaling to stimulate T-bet-mediated IFNγ production. Lack of genomic ADAM12 and its knockdown in T cells diminished T-bet and IFNγ production in Th1 cells, whereas other T cells, including Th17 cells, were unaffected. ADAM12 had similar functions in vivo on myelin antigen (MOG35-55)-induced T-cell activation. We found that genetic loss of ADAM12 profoundly alleviated Th1-mediated neuroinflammation and thus disease severity in experimental autoimmune encephalomyelitis, a model of multiple sclerosis. Transcriptomic profiling of MOG35-55-specific ADAM12-/- T cells revealed differentially expressed genes that are important for T-cell activation, proliferation, and costimulatory signaling and Th1 pathogenicity, consistent with their inability to cause T-cell-mediated skin inflammation in a model of adoptive delayed-type hypersensitivity. We conclude that ADAM12 is a T-cell costimulatory molecule that contributes to the pathogenesis of tissue inflammation and a potential target for the treatment of Th1-mediated diseases.
© 2020. The Author(s).
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
In Nat Commun on 24 April 2017 by Liu, Y., Marin, A., et al.
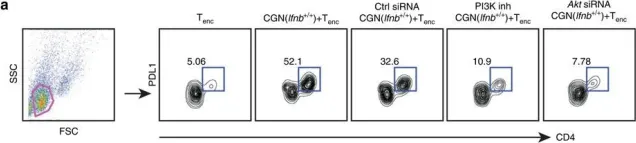
Fig.6.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 5
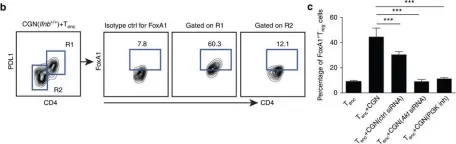
In Nat Commun on 24 April 2017 by Liu, Y., Marin, A., et al.
Fig.6.B

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 5
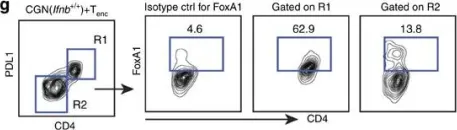
In Nat Commun on 24 April 2017 by Liu, Y., Marin, A., et al.
Fig.3.F

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 5
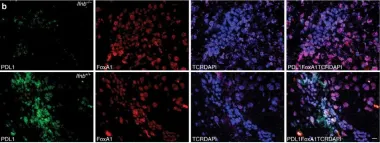
In Nat Commun on 24 April 2017 by Liu, Y., Marin, A., et al.
Fig.3.G

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 5
In Nat Commun on 24 April 2017 by Liu, Y., Marin, A., et al.
Fig.1.B

-
IF
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 5