Lymphocyte-specific protein tyrosine kinase (LCK) is essential for T cell antigen receptor (TCR)-mediated signal transduction. Here, we report two siblings homozygous for a novel LCK variant (c.1318C>T; P440S) characterized by T cell lymphopenia with skewed memory phenotype, infant-onset recurrent infections, failure to thrive, and protracted diarrhea. The patients' T cells show residual TCR signal transduction and proliferation following anti-CD3/CD28 and phytohemagglutinin (PHA) stimulation. We demonstrate in mouse models that complete (Lck-/-) versus partial (LckP440S/P440S) loss-of-function LCK causes disease with differing phenotypes. While both Lck-/- and LckP440S/P440S mice exhibit arrested thymic T cell development and profound T cell lymphopenia, only LckP440S/P440S mice show residual T cell proliferation, cytokine production, and intestinal inflammation. Furthermore, the intestinal disease in the LckP440S/P440S mice is prevented by CD4+ T cell depletion or regulatory T cell transfer. These findings demonstrate that P440S LCK spares sufficient T cell function to allow the maturation of some conventional T cells but not regulatory T cells-leading to intestinal inflammation.
© 2023 Lui et al.
Product Citations: 15
A partial human LCK defect causes a T cell immunodeficiency with intestinal inflammation.
In The Journal of Experimental Medicine on 1 January 2024 by Lui, V. G., Hoenig, M., et al.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
Dendritic cell expression of CD24 contributes to optimal priming of T lymphocytes in lymph nodes.
In Frontiers in Immunology on 28 March 2023 by Zhang, X., Yu, C., et al.
CD24 is a GPI anchored cell surface glycoprotein whose function as a co-stimulatory molecule has been implicated. However, the function of CD24 on antigen presenting cells during T cell responses is not well understood. Here we show that in the CD24-deficient host, adoptively transferred CD4+ T cells undergo inefficient expansion and have accelerated cell death in lymph nodes, which results in insufficient priming of T cells. Insufficient expansion of T cells in the CD24-deficient host was not due to host anti-CD24 response by NK, T and B lymphocytes. Transgenic expression of CD24 on DC in CD24-/- mice restored T cell accumulation and survival in draining lymph nodes. Consistent with these findings, MHC II tetramer staining also revealed that an antigen-specific polyclonal T cell response was reduced in lymph nodes of CD24-/- mice. Taken together, we have revealed a novel role of CD24 on DC in optimal T cell priming in lymph nodes. These data suggest that CD24 blockade should lower unwanted T cell responses such as those in autoimmune diseases.
Copyright © 2023 Zhang, Yu, Liu and Bai.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
Construction of a T cell receptor signaling range for spontaneous development of autoimmune disease.
In The Journal of Experimental Medicine on 6 February 2023 by Tanaka, A., Maeda, S., et al.
Thymic selection and peripheral activation of conventional T (Tconv) and regulatory T (Treg) cells depend on TCR signaling, whose anomalies are causative of autoimmunity. Here, we expressed in normal mice mutated ZAP-70 molecules with different affinities for the CD3 chains, or wild type ZAP-70 at graded expression levels under tetracycline-inducible control. Both manipulations reduced TCR signaling intensity to various extents and thereby rendered those normally deleted self-reactive thymocytes to become positively selected and form a highly autoimmune TCR repertoire. The signal reduction more profoundly affected Treg development and function because their TCR signaling was further attenuated by Foxp3 that physiologically repressed the expression of TCR-proximal signaling molecules, including ZAP-70, upon TCR stimulation. Consequently, the TCR signaling intensity reduced to a critical range generated pathogenic autoimmune Tconv cells and concurrently impaired Treg development/function, leading to spontaneous occurrence of autoimmune/inflammatory diseases, such as autoimmune arthritis and inflammatory bowel disease. These results provide a general model of how altered TCR signaling evokes autoimmune disease.
© 2022 Tanaka et al.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
Naïve arthritogenic SKG T cells have a defect in anergy and a repertoire pruned by superantigen
Preprint on BioRxiv : the Preprint Server for Biology on 16 January 2022 by Ashouri, J. F., McCarthy, E., et al.
How autoreactive CD4 T cells develop to cause rheumatoid arthritis remains unknown. We used a reporter for antigen-receptor signaling in the SKG autoimmune arthritis model to profile a T cell subpopulation enriched for arthritogenic naïve CD4 T cells before arthritis onset by bulk and single cell RNA and T cell antigen-receptor (TCR) sequencing. Our analyses reveal that despite their impaired proximal TCR signaling, a subset of SKG naïve CD4 T cells that have recently encountered endogenous antigen upregulate gene programs associated with positive regulation of T cell activation and cytokine signaling at higher levels than wild type cells in the pre-disease state. These arthritogenic cells also induce genes associated with negative regulation of T cell activation but do so less efficiently than wild type cells. Furthermore, their TCR sequences exhibit a previously unrecognized biased peripheral TCR Vβ repertoire likely driven by endogenous viral superantigens. These particular Vβs, known to recognize endogenous mouse mammary tumor virus (MMTV) superantigen, are further expanded in arthritic joints. Our results demonstrate that autoreactive naïve CD4 T cells which recognize endogenous viral superantigens are poised to cause disease by their altered transcriptome. h4>Summary blurb/h4> Self-reactive SKG T cells that escaped negative selection harbor an independent defect in anergy that, together with chronic antigen stimulation, sets the stage for disease. Moreover, we propose a novel role for endogenous mouse mammary tumor virus (MMTV) superantigen in promoting arthritogenic T cell responses.
-
Immunology and Microbiology
In Proceedings of the National Academy of Sciences of the United States of America on 30 March 2021 by Ronin, E., Pouchy, C., et al.
CD4+Foxp3+ regulatory T (Treg) cells are central modulators of autoimmune diseases. However, the timing and location of Treg cell-mediated suppression of tissue-specific autoimmunity remain undefined. Here, we addressed these questions by investigating the role of tumor necrosis factor (TNF) receptor 2 (TNFR2) signaling in Treg cells during experimental autoimmune encephalomyelitis (EAE), a model of multiple sclerosis. We found that TNFR2-expressing Treg cells were critical to suppress EAE at peak disease in the central nervous system but had no impact on T cell priming in lymphoid tissues at disease onset. Mechanistically, TNFR2 signaling maintained functional Treg cells with sustained expression of CTLA-4 and Blimp-1, allowing active suppression of pathogenic T cells in the inflamed central nervous system. This late effect of Treg cells was further confirmed by treating mice with TNF and TNFR2 agonists and antagonists. Our findings show that endogenous Treg cells specifically suppress an autoimmune disease by acting in the target tissue during overt inflammation. Moreover, they bring a mechanistic insight to some of the adverse effects of anti-TNF therapy in patients.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
In Front Immunol on 28 March 2023 by Zhang, X., Yu, C., et al.
Fig.5.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 5
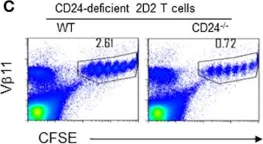
In Front Immunol on 28 March 2023 by Zhang, X., Yu, C., et al.
Fig.4.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 5
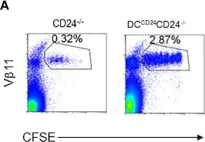
In Front Immunol on 28 March 2023 by Zhang, X., Yu, C., et al.
Fig.4.C

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 5
In Front Immunol on 28 March 2023 by Zhang, X., Yu, C., et al.
Fig.7.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 5
In Front Immunol on 28 March 2023 by Zhang, X., Yu, C., et al.
Fig.1.A

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 5