Allergic asthma features Th2-mediated airway inflammation, with dendritic cells (DCs) playing a crucial role. Acupuncture shows promise in modulating immune responses, yet its mechanisms in allergic asthma are not well understood. This study explores how acupuncture alleviates Th2 airway inflammation by modulating lung CD11b+ DCs.
Female BALB/c mice were assigned to control and asthma model groups, with subsets receiving acupuncture at Dazhui (GV14), Fengmen (BL12), and Feishu (BL13). We evaluated airway hyperresponsiveness (AHR), immune cell infiltration, histological changes, Th2 cytokine production, and serum IgE levels. The effects of acupuncture serum on T cell activation and bone marrow-derived dendritic cells (BMDCs) were assessed. The role of CD11b+ DCs was analyzed using flow cytometry, cytokine assays, and adoptive transfer experiments. Epithelial-derived alarmins and type 2 innate lymphoid cells (ILC2s) were also examined.
Acupuncture significantly reduced AHR, immune cell infiltration, goblet cell hyperplasia, and serum IgE levels in HDM-induced allergic asthma. It also suppressed Th2 cytokine production and differentiation. While acupuncture serum did not directly affect T cell activation, it modulated BMDC activity. Adoptive transfer of acupuncture-treated lung DCs into asthmatic mice reduced Th2 cell recruitment and ameliorated airway inflammation. Acupuncture reduced the population of lung CD11b+ DCs and downregulated the expression of activation markers such as CD86 and OX40L, along with Th2-promoting chemokines CCL17 and CCL22. Furthermore, it influenced CD11b+ DC migration by modulating CCR7, CCL2, and CCL8 expression. Acupuncture suppressed epithelial-derived alarmins IL-25, IL-33, and TSLP, attenuating ILC2 accumulation and activation, which indirectly affected CD11b+ DCs and Th2 responses.
Acupuncture alleviates Th2 airway inflammation in allergic asthma by modulating lung CD11b+ DC activities. These findings provide new insights into acupuncture-based therapeutic strategies for asthma.
© 2025. The Author(s).
Product Citations: 211
In Chinese Medicine on 22 May 2025 by Cheng, M., Shang, P. P., et al.
-
Immunology and Microbiology
Interleukin-4 modulates type I interferon to augment antitumor immunity.
In Science Advances on 16 May 2025 by Newnes, H. V., Armitage, J. D., et al.
Despite advances in immunotherapy, metastatic melanoma remains a considerable therapeutic challenge due to the complexity of the tumor microenvironment. Intratumoral type I interferon (IFN-I) has long been associated with improved clinical outcomes. However, several IFN-I subtypes can also paradoxically promote tumor growth in some contexts. We investigated this further by engineering murine B16 melanoma cells to overexpress various IFN-I subtypes, where a spectrum of outcomes was observed. Characterization of these tumors by RNA sequencing revealed a tumor immune phenotype, where potent IFN-I signaling concomitant with diminished type 2 inflammation failed to confer durable tumor control. T cell-mediated rejection of these tumors was restored by introducing interleukin-4 (IL-4) into the tumor microenvironment, either through ectopic expression or in a preclinical adoptive T cell therapy model. Collectively, our findings highlight the IFN-I/IL-4 axis in promoting antitumor immunity, which could be harnessed to target and stratify solid tumors that are nonresponsive to frontline therapies.
-
Immunology and Microbiology
In Nature Communications on 15 March 2025 by Khan, M., Alteneder, M., et al.
Lung pathogenic T helper type 2 (pTh2) cells are important in mediating allergic asthma, but fundamental questions remain regarding their heterogeneity and epigenetic regulation. Here we investigate immune regulation in allergic asthma by single-cell RNA sequencing in mice challenged with house dust mite, in the presence and absence of histone deacetylase 1 (HDAC1) function. Our analyses indicate two distinct highly proinflammatory subsets of lung pTh2 cells and pinpoint thymic stromal lymphopoietin (TSLP) and Tumour Necrosis Factor Receptor Superfamily (TNFRSF) members as important drivers to generate pTh2 cells in vitro. Using our in vitro model, we uncover how signalling via TSLP and a TNFRSF member shapes chromatin accessibility at the type 2 cytokine gene loci by modulating HDAC1 repressive function. In summary, we have generated insights into pTh2 cell biology and establish an in vitro model for investigating pTh2 cells that proves useful for discovering molecular mechanisms involved in pTh2-mediated allergic asthma.
© 2025. The Author(s).
Preprint on BioRxiv : the Preprint Server for Biology on 28 February 2025 by Lewis, D. A., Kar, A., et al.
Rapid proliferation and expansion of cytotoxic CD8 T lymphocytes is crucial for adaptive immunity against viral infection. CD8 T cell cycles complete cell division cycles in <6 hours, representing a physiological extreme for somatic mammalian cells. Embryonic stem cells also rapidly divide and have been shown to utilize specialized cell cycle control mechanisms that differ from somatic fibroblasts, including subdued periodicity of cyclin proteins. CD8 T cell cycle control remains poorly understood compared to embryonic and other somatic cell types. Here, we tested whether CD8 T cells utilize similar control mechanisms to embryonic stem cells to promote rapid cell cycles. We used mass spectrometry-based proteomics to comprehensively measure protein abundances in G1, S and G2&M phases somatic mouse CD8 T cells, mouse embryonic stem cells (mESC) and mouse fibroblasts (NIH3T3). We isolated cell cycle phases using PRIMMUS, thereby avoiding potential artefacts due to arrest-based synchronization. We discovered striking similarities between mESC and CD8 T cells. Similar to mESC, Cyclin E1 was expressed at high levels and constitutively across the cell cycle in CD8 T cells. Overall, cyclins and cell cycle regulated proteins were present in higher abundance in CD8 T cells and mESC as compared with NIH3T3 cells. Additionally, CD8 T cells express high levels of Emi1/Fbxo5 to promote S-phase entry. Interestingly, Emi1 deletion unexpectedly resulted in changes in markers of CD8 T cell phenotype, suggesting an association between cell cycle control and immune function. Thus, we show several adaptations of cell cycle control of embryonic stem cells are redeployed in somatic T cells to promote rapid cell cycles.
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
In Cell Death & Disease on 9 January 2025 by Chen, X., Zeng, Q., et al.
This research demonstrates that DCC-2036 (Rebastinib), a potent third-generation tyrosine kinase inhibitor (TKI), effectively suppresses tumor growth in colorectal cancer (CRC) models with functional immune systems. The findings underscore the capacity of DCC-2036 to enhance both the activation and cytotoxic functionality of CD8+ T cells, which are crucial for facilitating anti-tumor immune responses. Through comprehensive multi-omics investigations, significant shifts in both gene and protein expression profiles were detected, notably a marked decrease in DKK1 levels. This reduction in DKK1 was linked to diminished CD8+ T cell effectiveness, correlating with decreased FGR expression. Moreover, our findings identify FGR as a pivotal modulator that influences DKK1 expression via the PI3K-AKT-SP1 signaling cascade. Correlative analysis of clinical specimens supports the experimental data, showing that increased levels of FGR and DKK1 in CRC tissues are associated with inferior clinical outcomes and reduced efficacy of immunotherapeutic interventions. Consequently, targeting the FGR-AKT-SP1-DKK1 pathway with DCC-2036 could potentiate immunotherapy by enhancing CD8+ T cell functionality and their tumor infiltration. This strategy may contribute significantly to the refinement of therapeutic approaches for CRC, potentially improving patient prognoses.
© 2025. The Author(s).
-
Mus musculus (House mouse)
-
Cancer Research
-
Cell Biology
-
Immunology and Microbiology
In Front Immunol on 8 January 2025 by Raychaudhuri, K., Rangu, R., et al.
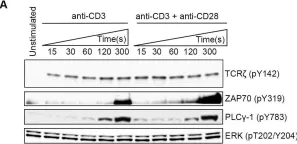
Fig.6.A

-
WB
-
Mus musculus (House mouse)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 2
In PLoS Pathog on 1 September 2022 by Iyer, R. F., Edwards, D. M., et al.
Fig.3.D

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from PLoS Pathog by CiteAb, provided under a CC-BY license
Image 1 of 2