Cyclosporin A (CSA) and tacrolimus (TAC) suppress T-cell activation and subsequent proliferation by inhibiting calcineurin. Though they have the same target, CSA and TAC have quite different molecular structures, indicating quantitative and/or qualitative differences in their effects.
CD28 is a costimulatory molecule that enhances T-cell activation. It has also been shown to attenuate calcineurin inhibitors. In this study, we compared the CD28-mediated resistance of CD4+ T cells to those calcineurin inhibitors and tried to predict CD28's impact on infectious diseases.
CD4+ T-cell proliferation was induced with anti-CD3 mAb in the presence or absence of anti-CD28 mAb in vitro. CSA or TAC was added at various concentrations, and the half-maximal inhibitory concentration on CD4+ T-cell proliferation was determined. Effects of lipopolysaccharide (LPS) on dendritic cells (DCs) and CD4+ T-cell proliferation were also evaluated in vitro.
Anti-CD28 mAb conferred CD4+ T cells with resistance to both CSA and TAC, and CD28's effect on the latter was approximately twice that on the former. LPS induced expression of CD28 ligands CD80/86 on DCs. The addition of LPS to culture containing DCs seemed to make CD4+ T cells slightly resistant to TAC but not to CSA. However, its effect on the former was very weak under our experimental conditions.
CD28 attenuated TAC more strongly than CSA. Although LPS did not demonstrate strong enough resistance in our in vitro model, TAC might maintain a better antibacterial immune response than CSA in clinical use.
Product Citations: 28
CD28 confers CD4+ T cells with resistance to cyclosporin A and tacrolimus but to different degrees.
In Asian Pacific Journal of Allergy and Immunology / Launched By the Allergy and Immunology Society of Thailand on 1 September 2024 by Kawai, H., Yagyu, F., et al.
-
Immunology and Microbiology
An mRNA vaccine elicits STING-dependent antitumor immune responses.
In Acta Pharmaceutica Sinica. B on 1 March 2023 by Chen, Z., Meng, C., et al.
Lipid-formulated RNA vaccines have been widely used for disease prevention and treatment, yet their mechanism of action and individual components contributing to such actions remain to be delineated. Here, we show that a therapeutic cancer vaccine composed of a protamine/mRNA core and a lipid shell is highly potent in promoting cytotoxic CD8+ T cell responses and mediating anti-tumor immunity. Mechanistically, both the mRNA core and lipid shell are needed to fully stimulate the expression of type I interferons and inflammatory cytokines in dendritic cells. Stimulation of interferon-β expression is exclusively dependent on STING, and antitumor activity from the mRNA vaccine is significantly compromised in mice with a defective Sting gene. Thus, the mRNA vaccine elicits STING-dependent antitumor immunity.
© 2022 Chinese Pharmaceutical Association and Institute of Materia Medica, Chinese Academy of Medical Sciences. Production and hosting by Elsevier B.V.
-
WB
-
Mus musculus (House mouse)
-
Genetics
-
Immunology and Microbiology
In Cell Reports on 31 March 2020 by Muri, J., Feng, Q., et al.
Oxidized lipids play a critical role in a variety of diseases with two faces: pro- and anti-inflammatory. The molecular mechanisms of this Janus-faced activity remain largely unknown. Here, we have identified that cyclopentenone-containing prostaglandins such as 15d-PGJ2 and structurally related oxidized phospholipid species possess a dual and opposing bioactivity in inflammation, depending on their concentration. Exposure of dendritic cells (DCs)/macrophages to low concentrations of such lipids before Toll-like receptor (TLR) stimulation instigates an anti-inflammatory response mediated by nuclear factor erythroid 2-related factor 2 (Nrf2)-dependent inhibition of nuclear factor κB (NF-κB) activation and downstream targets. By contrast, high concentrations of such lipids upon TLR activation of DCs/macrophages result in inflammatory apoptosis characterized by mitochondrial depolarization and caspase-8-mediated interleukin (IL)-1β maturation independently of Nrf2 and the classical inflammasome pathway. These results uncover unexpected pro- and anti-inflammatory activities of physiologically relevant lipid species generated by enzymatic and non-enzymatic oxidation dependent on their concentration, a phenomenon known as hormesis.Copyright © 2020 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Immunology and Microbiology
The cytokine network type I IFN-IL-27-IL-10 is augmented in murine and human lupus.
In Journal of Leukocyte Biology on 1 October 2019 by Lee, M. H., Gallo, P. M., et al.
IL-10 is elevated in the autoimmune disease systemic lupus erythematosus (SLE). Here, we show that conventional dendritic cells (cDCs) from predisease lupus-prone B6.NZM Sle1/Sle2/Sle3 triple congenic (TCSle) mice produce more IL-10 than wild-type congenic cDCs upon TLR stimulation, and this overproduction is prevented by blocking the type I IFN receptor (IFNAR) with specific Abs. Priming wild-type cDCs with type I IFN mimics the IL-10 overproduction of TCSle cDCs. The MAPK ERK is more phosphorylated in lupus cDCs, partially contributing to IL-10 overproduction. Moreover, we found that TCSle cDCs express higher levels of IL-27 upon TLR7/TLR9 stimulation, and IFNAR blockade reduced IL-27 levels in TCSle cDCs. These results suggest that dysregulated type I IFNs in cDCs contribute to the increased IL-10 and IL-27 in SLE. Since IL-27 neutralization did not inhibit TLR-induced IL-10 production, we propose that type I IFNs enhanced IL-10 in TCSle cDCs independently from IL-27. Moreover, RNA sequencing analysis of a cohort of SLE patients reveals higher gene expression of these cytokines in SLE patients expressing a high IFN signature. Since IL-27 and IL-10 have both pro- and anti-inflammatory effects, our results also suggest that these cytokines can be modulated by the therapeutic IFN blockade in trials in SLE patients and have complex effects on the autoimmune response.
©2019 Society for Leukocyte Biology.
-
Immunology and Microbiology
Intratumoral injection of dendritic cells overexpressing interleukin‑12 inhibits melanoma growth.
In Oncology Reports on 1 July 2019 by Yao, W., Li, Y., et al.
The present study aimed to investigate the antitumor effects of an intratumoral injection of dendritic cells (DCs) overexpressing interleukin-12 (IL‑12) on melanoma. DCs, isolated from mouse spleen, were gene‑modified using an IL‑12 overexpression vector. Melanoma B6 cells were injected into C57BL/6 mice to generate tumors. Thereafter, DCs overexpressing IL‑12 were injected into the tumors, and tumor volume was subsequently measured. Pathological changes in tumor tissue were detected by hematoxylin and eosin staining. The expression of interleukin-4 (IL‑4) and IL‑12 in tumors was measured by enzyme‑linked immunosorbent assay, real‑time PCR and western blotting. DCs were successfully isolated and a lentivirus vector expressing IL‑12 was constructed. After intratumoral injection of phosphate‑buffered saline (control group), tumor cells exhibited malignant growth; whereas tumors injected with DCs (DC group) or DCs + empty vector (DC + vector group) exhibited a small amount of inflammatory cell infiltration and limited areas of tissue necrosis. In contrast, tumors injected with DCs overexpressing IL‑12 (DC + IL‑12 group) displayed severe tissue necrosis, loss of cell structure, and inflammatory cell infiltration. Compared with the control group, the tumor volumes were significantly lower in the DC, the DC + vector and the DC + IL‑12 groups, while the expression of IL‑12 and IL‑4 in the tumors was significantly higher. Importantly, the most marked changes in tumor volume and IL‑12 and IL‑4 expression were in the DC + IL‑12 group, which were significantly greater than those in tumors treated with unmodified DCs. Hence, intratumoral injection of DCs overexpressing IL‑12 exerted strong antitumor effects in melanoma, and biotherapy with DCs overexpressing IL‑12 is a potential treatment strategy for melanoma.
-
Cancer Research
-
Immunology and Microbiology
In PLoS One on 21 May 2015 by Abd Warif, N. M., Stoitzner, P., et al.
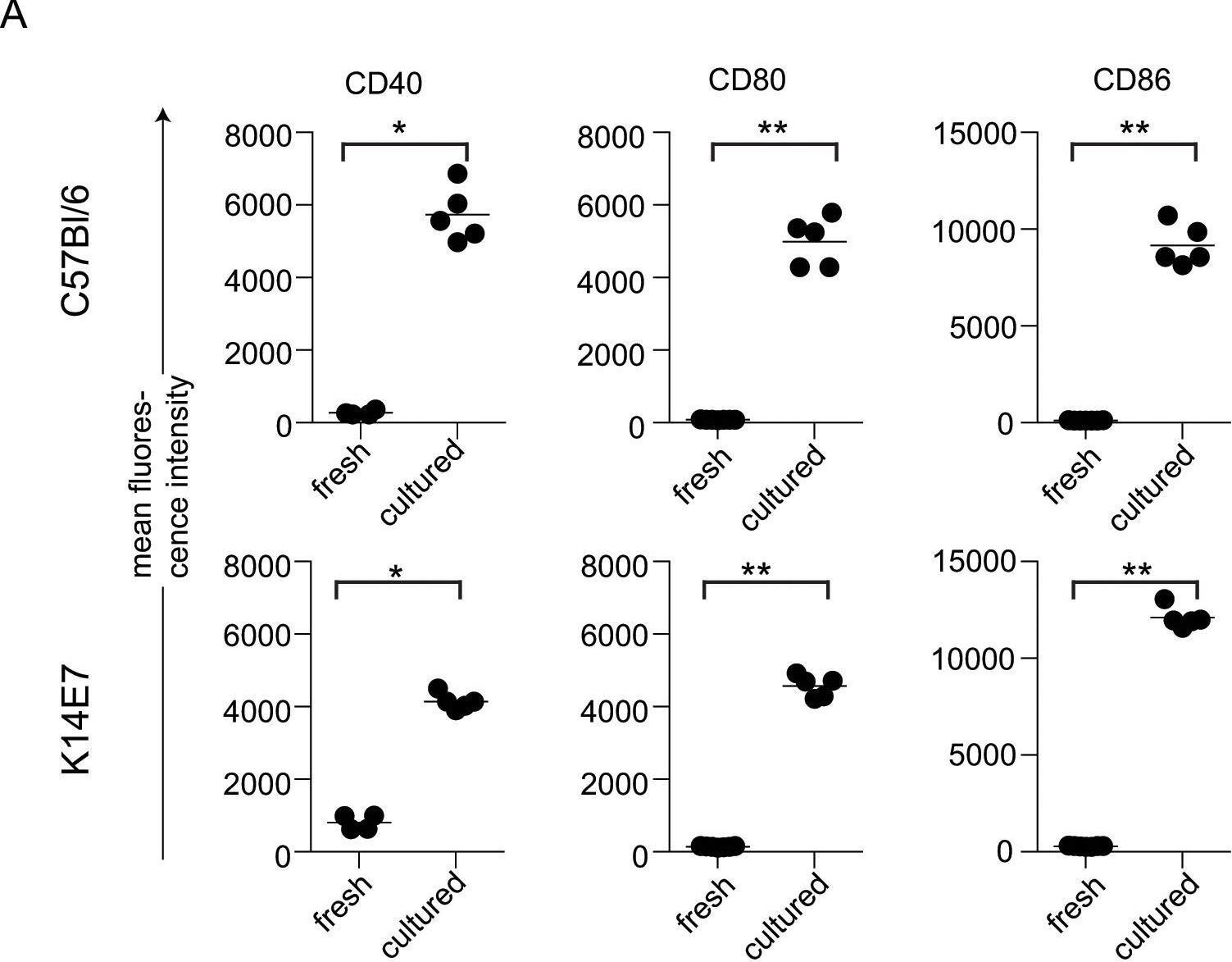
Fig.6.A
-
FC/FACS
-
Collected and cropped from PLoS ONE by CiteAb, provided under a CC-BY license
Image 1 of 1
