Medullary thymic epithelial cells (mTEC) are bona fide antigen-presenting cells that play a crucial role in the induction of T-cell tolerance. By their unique ability to express a broad range of tissue-restricted self-antigens, mTEC control the clonal deletion (also known as negative selection) of potentially hazardous autoreactive T cells and the generation of Foxp3+ regulatory T cells. Here, we describe a protocol to assess major histocompatibility complex (MHC) class II antigen-presentation capacity of mTEC to CD4+ T cells. We detail the different steps of thymus enzymatic digestion, immunostaining, cell sorting of mTEC and CD4+ T cells, peptide-loading of mTEC, and the co-culture between these two cell types. Finally, we describe the flow cytometry protocol and the subsequent analysis to assess the activation of CD4+ T cells. This rapid co-culture assay enables the evaluation of the ability of mTEC to present antigens to CD4+ T cells in an antigen-specific context. Key features • This protocol builds upon the method used by Lopes et al. (2018 and 2022) and Charaix et al. (2022). • This protocol requires transgenic mice, such as OTIIxRag2-/- mice and the cognate peptide OVA323-339, to assess mTEC antigen presentation to CD4+ T cells. • This requires specific equipment such as a Miltenyi Biotec AutoMACS® Pro Separator, a BD FACSAriaTM III cell sorter, and a BD® LSR II flow cytometer.
©Copyright : © 2023 The Authors; This is an open access article under the CC BY license.
Product Citations: 21
Medullary Thymic Epithelial Cell Antigen-presentation Assays.
In Bio-protocol on 5 November 2023 by Borelli, A., Zamit, C., et al.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
The histone H2B ubiquitination regulator Wac is essential for plasma cell differentiation.
In FEBS Letters on 1 July 2023 by Li, Y., Ruan, G. X., et al.
Naïve B cells become activated and differentiate into antibody-secreting plasma cells (PCs) when encountering antigens. Here, we reveal that the WW domain-containing adapter protein with coiled-coil (Wac), which is important for histone H2B ubiquitination (ubH2B), is essential for PC differentiation. We demonstrate that B cell-specific Wac knockout mice have severely compromised T cell-dependent and -independent antibody responses. PC differentiation is drastically compromised despite undisturbed germinal center B cell response in the mutant mice. We also observe a significant reduction in global ubH2B in Wac-deficient B cells, which is correlated with downregulated expression of some genes critical for cell metabolism. Thus, our findings demonstrate an essential role of Wac-mediated ubH2B in PC differentiation and shed light on the epigenetic mechanisms underlying this process.
© 2023 Federation of European Biochemical Societies.
-
FC/FACS
-
Mus musculus (House mouse)
-
Genetics
Prolidase Deficiency Causes Spontaneous T Cell Activation and Lupus-like Autoimmunity.
In The Journal of Immunology on 1 March 2023 by Hodgson, R., Crockford, T. L., et al.
Prolidase deficiency (PD) is a multisystem disorder caused by mutations in the PEPD gene, which encodes a ubiquitously expressed metallopeptidase essential for the hydrolysis of dipeptides containing C-terminal proline or hydroxyproline. PD typically presents in childhood with developmental delay, skin ulcers, recurrent infections, and, in some patients, autoimmune features that can mimic systemic lupus erythematosus. The basis for the autoimmune association is uncertain, but might be due to self-antigen exposure with tissue damage, or indirectly driven by chronic infection and microbial burden. In this study, we address the question of causation and show that Pepd-null mice have increased antinuclear autoantibodies and raised serum IgA, accompanied by kidney immune complex deposition, consistent with a systemic lupus erythematosus-like disease. These features are associated with an accumulation of CD4 and CD8 effector T cells in the spleen and liver. Pepd deficiency leads to spontaneous T cell activation and proliferation into the effector subset, which is cell intrinsic and independent of Ag receptor specificity or antigenic stimulation. However, an increase in KLRG1+ effector CD8 cells is not observed in mixed chimeras, in which the autoimmune phenotype is also absent. Our findings link autoimmune susceptibility in PD to spontaneous T cell dysfunction, likely to be acting in combination with immune activators that lie outside the hemopoietic system but result from the abnormal metabolism or loss of nonenzymatic prolidase function. This knowledge provides insight into the role of prolidase in the maintenance of self-tolerance and highlights the importance of treatment to control T cell activation.
Copyright © 2023 The Authors.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
NDRG1 is induced by antigen-receptor signaling but dispensable for B and T cell self-tolerance.
In Communications Biology on 10 November 2022 by Hodgson, R., Xu, X., et al.
Peripheral tolerance prevents the initiation of damaging immune responses by autoreactive lymphocytes. While tolerogenic mechanisms are tightly regulated by antigen-dependent and independent signals, downstream pathways are incompletely understood. N-myc downstream-regulated gene 1 (NDRG1), an anti-cancer therapeutic target, has previously been implicated as a CD4+ T cell clonal anergy factor. By RNA-sequencing, we identified Ndrg1 as the third most upregulated gene in anergic, compared to naïve follicular, B cells. Ndrg1 is upregulated by B cell receptor activation (signal one) and suppressed by co-stimulation (signal two), suggesting that NDRG1 may be important in B cell tolerance. However, though Ndrg1-/- mice have a neurological defect mimicking NDRG1-associated Charcot-Marie-Tooth (CMT4d) disease, primary and secondary immune responses were normal. We find that B cell tolerance is maintained, and NDRG1 does not play a role in downstream responses during re-stimulation of in vivo antigen-experienced CD4+ T cells, demonstrating that NDGR1 is functionally redundant for lymphocyte anergy.
© 2022. The Author(s).
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
In The Journal of Immunology on 1 April 2022 by Wemlinger, S. M., Parker Harp, C. R., et al.
The BCR comprises a membrane-bound Ig that is noncovalently associated with a heterodimer of CD79A and CD79B. While the BCR Ig component functions to sense extracellular Ag, CD79 subunits contain cytoplasmic ITAMs that mediate intracellular propagation of BCR signals critical for B cell development, survival, and Ag-induced activation. CD79 is therefore an attractive target for Ab and chimeric Ag receptor T cell therapies for autoimmunity and B cell neoplasia. Although the mouse is an attractive model for preclinical testing, due to its well-defined immune system, an obstacle is the lack of cross-reactivity of candidate therapeutic anti-human mAbs with mouse CD79. To overcome this problem, we generated knockin mice in which the extracellular Ig-like domains of CD79A and CD79B were replaced with human equivalents. In this study, we describe the generation and characterization of mice expressing chimeric CD79 and report studies that demonstrate their utility in preclinical analysis of anti-human CD79 therapy. We demonstrate that human and mouse CD79 extracellular domains are functionally interchangeable, and that anti-human CD79 lacking Fc region effector function does not cause significant B cell depletion, but induces 1) decreased expression of plasma membrane-associated IgM and IgD, 2) uncoupling of BCR-induced tyrosine phosphorylation and calcium mobilization, and 3) increased expression of PTEN, consistent with the levels observed in anergic B cells. Finally, anti-human CD79 treatment prevents disease development in two mouse models of autoimmunity. We also present evidence that anti-human CD79 treatment may inhibit Ab secretion by terminally differentiated plasmablasts and plasma cells in vitro.Copyright © 2022 by The American Association of Immunologists, Inc.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
In Sci Rep on 25 May 2017 by Yin, C., Pei, X. Y., et al.
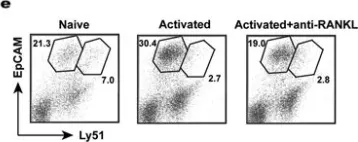
Fig.5.E

-
FC/FACS
-
Collected and cropped from Sci Rep by CiteAb, provided under a CC-BY license
Image 1 of 1