Immune checkpoint blockade (ICB) therapies are an important treatment for patients with advanced cancers; however, only a subset of patients with certain types of cancer achieve durable remission. Cancer vaccines are an attractive strategy to boost patient immune responses, but less is known about whether and how immunization can induce long-term tumor immune reprogramming and arrest cancer progression. We developed a clinically relevant genetic cancer mouse model in which hepatocytes sporadically undergo oncogenic transformation. We compared how tumor-specific CD8 T cells (TST) differentiated in mice with early sporadic lesions as compared with late lesions and tested how immunotherapeutic strategies, including vaccination and ICB, impact TST function and liver cancer progression.
Mice with a germline floxed allele of the SV40 large T antigen (TAG) undergo spontaneous recombination and activation of the TAG oncogene, leading to rare early cancerous TAG-expressing lesions that inevitably progress to established liver cancer. We assessed the immunophenotype (CD44, PD1, TCF1, and TOX expression) and function (TNFα and IFNγ cytokine production) of tumor/TAG-specific CD8 T cells in mice with early and late liver lesions by flow cytometry. We vaccinated mice, either alone or in combination with ICB, to test whether these immunotherapeutic interventions could stop liver cancer progression and improve survival.
In mice with early lesions, a subset of TST were PD1+ TCF1+ TOX- and could produce IFNγ while TST present in mice with late liver cancers were PD1+ TCF1lo/- TOX+ and unable to make effector cytokines. Strikingly, vaccination with attenuated TAG epitope-expressing Listeria monocytogenes (LMTAG) blocked liver cancer development and led to a population of TST that were PD1-heterogeneous, TCF1+ TOX- and polyfunctional cytokine producers. Vaccine-elicited TCF1+TST could self-renew and differentiate, establishing them as progenitor TST. In contrast, ICB administration did not slow cancer progression or improve LMTAG vaccine efficacy.
Vaccination, but not ICB, generated a population of functional progenitor TST and halted cancer progression in a clinically relevant model of sporadic liver cancer. In patients with early cancers or at high risk of cancer recurrence, immunization may be the most effective strategy.
© Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Product Citations: 30
Vaccination generates functional progenitor tumor-specific CD8 T cells and long-term tumor control.
In Journal for Immunotherapy of Cancer on 3 October 2024 by Detrés Román, C. R., Erwin, M. M., et al.
-
Cancer Research
-
Immunology and Microbiology
Histone demethylase PHF8 promotes prostate cancer metastasis via the E2F1-SNAI1 axis.
In The Journal of Pathology on 1 September 2024 by Wang, Z., Tang, P., et al.
Metastasis is the primary culprit behind cancer-related fatalities in multiple cancer types, including prostate cancer. Despite great advances, the precise mechanisms underlying prostate cancer metastasis are far from complete. By using a transgenic mouse prostate cancer model (TRAMP) with and without Phf8 knockout, we have identified a crucial role of PHF8 in prostate cancer metastasis. By complexing with E2F1, PHF8 transcriptionally upregulates SNAI1 in a demethylation-dependent manner. The upregulated SNAI1 subsequently enhances epithelial-to-mesenchymal transition (EMT) and metastasis. Given the role of the abnormally activated PHF8/E2F1-SNAI1 axis in prostate cancer metastasis and poor prognosis, the levels of PHF8 or the activity of this axis could serve as biomarkers for prostate cancer metastasis. Moreover, targeting this axis could become a potential therapeutic strategy for prostate cancer treatment. © 2024 The Pathological Society of Great Britain and Ireland.
© 2024 The Pathological Society of Great Britain and Ireland.
-
IHC
-
Cancer Research
-
Genetics
-
Pathology
Vaccination generates functional progenitor tumor-specific CD8 T cells and long-term tumor control
Preprint on BioRxiv : the Preprint Server for Biology on 29 February 2024 by Detrés Román, C. R., Rudloff, M. W., et al.
ABSTRACT Background Immune checkpoint blockade (ICB) therapies are an important treatment for patients with advanced cancers; however only a subset of patients with certain types of cancer achieves durable remissions. Cancer vaccines are an attractive strategy to boost patient immune responses, but less is known about whether and how immunization can induce long-term tumor immune reprogramming and arrest cancer progression. We developed a clinically-relevant genetic cancer mouse model in which hepatocytes sporadically undergo oncogenic transformation. We compared how tumor-specific CD8 T cells (TST) differentiate in mice with early sporadic lesions as compared to late lesions and tested how immunotherapeutic strategies, including vaccination and ICB, reprogram TST and impact liver cancer progression. Methods Mice with a germline floxed allele of the SV40 large T antigen (TAG) undergo spontaneous recombination and activation of the TAG oncogene, leading to rare early pre-cancerous lesions that inevitably progress to established liver cancer. We assessed the immunophenotype and function of TAG-specific CD8 T cells in mice with early and late liver lesions. We vaccinated mice, either alone or in combination with ICB, to test whether these immunotherapeutic interventions could stop liver cancer progression. Results In mice with early lesions, a subset of TST were PD1 + TCF1 + TOX - and could produce IFNγ, while TST present in mice with late liver cancers were PD1 + TCF1 lo/- TOX + and unable to make effector cytokines. Strikingly, vaccination with attenuated TAG epitope-expressing Listeria monocytogenes (LM TAG ) blocked liver cancer development and led to a population of TST that were TCF1 + TOX - TST and polyfunctional cytokine producers. In contrast, ICB administration did not slow cancer progression or improve LM TAG vaccine efficacy. Conclusion Vaccination, but not ICB, generated a population of progenitor TST and halted cancer progression in a clinically relevant model of sporadic liver cancer. In patients with early cancers or at high-risk of cancer recurrence, immunization may be the most effective strategy. What is already known on this topic Immunotherapy, including immune checkpoint blockade and cancer vaccines, fails to induce long-term remissions in most patients with cancer. What this study adds Hosts with early lesions but not hosts with advanced cancer retain a progenitor TCF1+ TST population. This population can be reprogrammed and therapeutically exploited by vaccination, but not ICB, to block tumor progression. How this study might affect research, practice, or policy For people at high-risk of cancer progression, vaccination administered when a responsive progenitor TST population is present may be the optimal immunotherapy to induce long-lasting progression-free survival.
-
Cancer Research
-
Immunology and Microbiology
Deregulated expression of the 14q32 miRNA cluster in clear cell renal cancer cells.
In Frontiers in Oncology on 4 May 2023 by Chhabra, R., Guergues, J., et al.
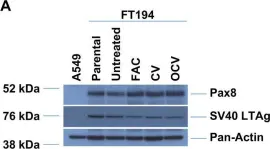
Clear cell renal cell carcinomas (ccRCC) are characterized by arm-wide chromosomal alterations. Loss at 14q is associated with disease aggressiveness in ccRCC, which responds poorly to chemotherapeutics. The 14q locus contains one of the largest miRNA clusters in the human genome; however, little is known about the contribution of these miRNAs to ccRCC pathogenesis. In this regard, we investigated the expression pattern of selected miRNAs at the 14q32 locus in TCGA kidney tumors and in ccRCC cell lines. We demonstrated that the miRNA cluster is downregulated in ccRCC (and cell lines) as well as in papillary kidney tumors relative to normal kidney tissues (and primary renal proximal tubule epithelial (RPTEC) cells). We demonstrated that agents modulating expression of DNMT1 (e.g., 5-Aza-deoxycytidine) could modulate 14q32 miRNA expression in ccRCC cell lines. Lysophosphatidic acid (LPA, a lysophospholipid mediator elevated in ccRCC) not only increased labile iron content but also modulated expression of a 14q32 miRNA. Through an overexpression approach targeting a subset of 14q32 miRNAs (specifically at subcluster A: miR-431-5p, miR-432-5p, miR-127-3p, and miR-433-3p) in 769-P cells, we uncovered changes in cellular viability and claudin-1, a tight junction marker. A global proteomic approach was implemented using these miRNA overexpressing cell lines which uncovered ATXN2 as a highly downregulated target. Collectively, these findings support a contribution of miRNAs at 14q32 in ccRCC pathogenesis.
Copyright © 2023 Chhabra, Guergues, Wohlfahrt, Rockfield, Espinoza Gonzalez, Rego, Park, Berglund, Stevens and Nanjundan.
-
WB
-
Cancer Research
-
Genetics
In NPJ Breast Cancer on 11 May 2021 by Stanton, S. E., Gad, E., et al.
B cell responses to tumor antigens occur early in breast tumors and may identify immunogenic drivers of tumorigenesis. Sixty-two candidate antigens were identified prior to palpable tumor development in TgMMTV-neu and C3(1)Tag transgenic mouse mammary tumor models. Five antigens (VPS35, ARPC2, SERBP1, KRT8, and PDIA6) were selected because their decreased expression decreased survival in human HER2 positive and triple negative cell lines in a siRNA screen. Vaccination with antigen-specific epitopes, conserved between mouse and human, inhibited tumor growth in both transgenic mouse models. Increased IgG autoantibodies to the antigens were elevated in serum from women with ductal carcinoma in situ (DCIS) and invasive breast cancer (IBC). The autoantibodies differentiated women with DCIS from control with AUC 0.93 (95% CI 0.88-0.98, p < 0.0001). The tumor antigens identified early in the development of breast cancer in mouse mammary tumor models were conserved in human disease, and potentially identify early diagnostic markers in human breast tumors.
-
Cancer Research
In Oncogenesis on 21 August 2019 by Rockfield, S., Kee, Y., et al.
Fig.5.A

-
WB
-
Collected and cropped from Oncogenesis by CiteAb, provided under a CC-BY license
Image 1 of 1