Liver sinusoidal endothelial cells (LSECs) which make up the fenestrated wall of the hepatic sinusoids, are active scavenger cells involved in blood waste clearance and liver immune functions. Dexamethasone is a synthetic glucocorticoid commonly used in the clinic and as cell culture supplement. However, the response is dependent on tissue, cell type, and cell state. The aim of this study was to investigate the effect of dexamethasone on primary mouse LSECs (C57BL/6J); their viability (live-dead, LDH release, caspase 3/7 assays), morphology (scanning electron microscopy), release of inflammatory markers (ELISA), and scavenging functions (endocytosis assays), and associated biological processes and pathways. We have characterized and catalogued the proteome of LSECs cultured for 1, 10, or 48 h to elucidate time-dependent and dexamethasone-specific cell responses. More than 6,000 protein IDs were quantified using tandem mass tag technology and advanced mass spectrometry (synchronous precursor selection multi-notch MS3). Enrichment analysis showed a culture-induced upregulation of stress and inflammatory markers, and a significant shift in cell metabolism already at 10 h, with enhancement of glycolysis and concomitant repression of oxidative phosphorylation. At 48 h, changes in metabolic pathways were more pronounced with dexamethasone compared to time-matched controls. Dexamethasone repressed the activation of inflammatory pathways (IFN-gamma response, TNF-alpha signaling via NF-kB, Cell adhesion molecules), and culture-induced release of interleukin-6, VCAM-1, and ICAM-1, and improved cell viability partly through inhibition of apoptosis. The mouse LSECs did not proliferate in culture. Dexamethasone treated cells showed upregulation of xanthine dehydrogenase/oxidase (Xdh), and the transcription regulator Foxo1. The drug further delayed but did not block the culture-induced loss of LSEC fenestration. The LSEC capacity for endocytosis was significantly reduced at 48 h, independent of dexamethasone, which correlated with diminished expression of several scavenger receptors and C-type lectins and altered expression of proteins in the endocytic machinery. The glucocorticoid receptor (NR3C1) was suppressed by dexamethasone at 48 h, suggesting limited effect of the drug in prolonged LSEC culture. Conclusion: The study presents a detailed overview of biological processes and pathways affected by dexamethasone in mouse LSECs in vitro.
Copyright © 2024 Bhandari, Kyrrestad, Simón-Santamaría, Li, Szafranska, Dumitriu, Sánchez Romano, Smedsrød and Sørensen.
Product Citations: 181
In Frontiers in Pharmacology on 23 October 2024 by Bhandari, S., Kyrrestad, I., et al.
-
Mus musculus (House mouse)
-
Pharmacology
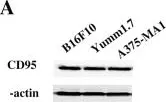
The abscopal effect of anti-CD95 and radiotherapy in melanoma.
In Discov Oncol on 16 May 2023 by Xu, J., He, J., et al.
Radiotherapy (RT) is frequently adopted to control cancer cell proliferation, which is achieved by altering the tumor microenvironment (TME) and immunogenicity. Apoptosis of cancer cells is the major effect of radiation on tumor tissues. Fas/APO-1(CD95) receptors on the cell membrane are death receptors that can be activated by diverse factors, including radiation and integration with CD95L on CD8+ T cells. The abscopal effect is defined as tumor regression out of the local RT field, and it is produced through anti-tumor immunity. The immune response against the radiated tumor is characterized by the cross-presentation between antigen-presenting cells (APCs), which includes cytotoxic T cells (CTLs) and dendritic cells (DCs).
The effect of activation and radiation of CD95 receptors on melanoma cell lines was examined in vivo and in vitro. In vivo, bilateral lower limbs were given a subcutaneous injection of a dual-tumor. Tumors in the right limb were radiated with a single dose of 10 Gy (primary tumor), while tumors in the left limb (secondary tumor) were spared.
The anti-CD95 treatment plus radiation (combination treatment) reduced growth rates of both primary and secondary tumors relative to the control or radiation groups. In addition, higher degrees of infiltrating CTLs and DCs were detected in the combination treatment compared to the other groups, but the immune response responsible for secondary tumor rejection was not proven to be tumor specific. In vitro, combination treatment combined with radiation resulted in further apoptosis of melanoma cells relative to controls or cells treated with radiation.
Targeting CD95 on cancer cells will induce tumor control and the abscopal effect.
© 2023. The Author(s).
-
WB
-
Cancer Research
Myeloid TLR4 signaling promotes post-injury withdrawal resolution of murine liver fibrosis.
In IScience on 17 March 2023 by Takimoto, Y., Chu, P. S., et al.
The fate of resolution of liver fibrosis after withdrawal of liver injury is still incompletely elucidated. Toll-like receptor 4 (TLR4) in tissue fibroblasts is pro-fibrogenic. After withdrawal of liver injury, we unexpectedly observed a significant delay of fibrosis resolution as TLR4 signaling was pharmacologically inhibited in vivo in two murine models. Single-cell transcriptome analysis of hepatic CD11b+ cells, main producers of matrix metalloproteinases (MMPs), revealed a prominent cluster of restorative Tlr4-expressing Ly6c2-low myeloid cells. Delayed resolution after gut sterilization suggested its microbiome-dependent nature. Enrichment of a metabolic pathway linking to a significant increase of bile salt hydrolase-possessing family Erysipelotrichaceae during resolution. Farnesoid X receptor-stimulating secondary bile acids including 7-oxo-lithocholic acids upregulated MMP12 and TLR4 in myeloid cells in vitro. Fecal material transplant in germ-free mice confirmed phenotypical correlations in vivo. These findings highlight a pro-fibrolytic role of myeloid TLR4 signaling after injury withdrawal and may provide targets for anti-fibrotic therapy.
© 2023 The Author(s).
-
Mus musculus (House mouse)
Opposing roles of hepatic stellate cell subpopulations in hepatocarcinogenesis.
In Nature on 1 October 2022 by Filliol, A., Saito, Y., et al.
Hepatocellular carcinoma (HCC), the fourth leading cause of cancer mortality worldwide, develops almost exclusively in patients with chronic liver disease and advanced fibrosis1,2. Here we interrogated functions of hepatic stellate cells (HSCs), the main source of liver fibroblasts3, during hepatocarcinogenesis. Genetic depletion, activation or inhibition of HSCs in mouse models of HCC revealed their overall tumour-promoting role. HSCs were enriched in the preneoplastic environment, where they closely interacted with hepatocytes and modulated hepatocarcinogenesis by regulating hepatocyte proliferation and death. Analyses of mouse and human HSC subpopulations by single-cell RNA sequencing together with genetic ablation of subpopulation-enriched mediators revealed dual functions of HSCs in hepatocarcinogenesis. Hepatocyte growth factor, enriched in quiescent and cytokine-producing HSCs, protected against hepatocyte death and HCC development. By contrast, type I collagen, enriched in activated myofibroblastic HSCs, promoted proliferation and tumour development through increased stiffness and TAZ activation in pretumoural hepatocytes and through activation of discoidin domain receptor 1 in established tumours. An increased HSC imbalance between cytokine-producing HSCs and myofibroblastic HSCs during liver disease progression was associated with increased HCC risk in patients. In summary, the dynamic shift in HSC subpopulations and their mediators during chronic liver disease is associated with a switch from HCC protection to HCC promotion.
© 2022. The Author(s), under exclusive licence to Springer Nature Limited.
In Cell Death and Differentiation on 1 August 2022 by Li, X., Li, F., et al.
Caspase-8 is an initiator of death receptor-induced apoptosis and an inhibitor of RIPK3-MLKL-dependent necroptosis. In addition, caspase-8 has been implicated in diseases such as lymphoproliferation, immunodeficiency, and autoimmunity in humans. Although auto-cleavage is indispensable for caspase-8 activation, its physiological functions remain poorly understood. Here, we generated a caspase-8 mutant lacking E385 in auto-cleavage site knock-in mouse (Casp8ΔE385/ΔE385). Casp8ΔE385/ΔE385 cells were expectedly resistant to Fas-induced apoptosis, however, Casp8ΔE385/ΔE385 cells could switch TNF-α-induced apoptosis to necroptosis by attenuating RIPK1 cleavage. More importantly, CASP8(ΔE385) sensitized cells to RIPK3-MLKL-dependent necroptosis through promoting complex II formation and RIPK1-RIPK3 activation. Notably, Casp8ΔE385/ΔE385Ripk3-/- mice partially rescued the perinatal death of Ripk1-/- mice by blocking apoptosis and necroptosis. In contrast to the Casp8-/-Ripk3-/- and Casp8-/-Mlkl-/- mice appearing autoimmune lymphoproliferative syndrome (ALPS), both Casp8ΔE385/ΔE385Ripk3-/- and Casp8ΔE385/ΔE385Mlkl-/- mice developed transplantable lymphopenia that could be significantly reversed by RIPK1 heterozygosity, but not by RIPK1 kinase dead mutation. Collectively, these results demonstrate previously unappreciated roles for caspase-8 auto-cleavage in regulating necroptosis and maintaining lymphocytes homeostasis.
© 2022. The Author(s), under exclusive licence to ADMC Associazione Differenziamento e Morte Cellulare.
-
FC/FACS
-
Mus musculus (House mouse)
-
Cell Biology
In Discov Oncol on 16 May 2023 by Xu, J., He, J., et al.
Fig.1.A

-
WB
-
Collected and cropped from Discov Oncol by CiteAb, provided under a CC-BY license
Image 1 of 7
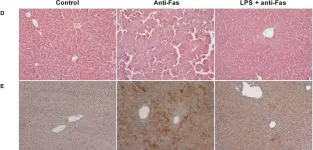
In J Cell Mol Med on 1 March 2020 by Markotic, A., Flegar, D., et al.
Fig.1.D

-
IHC
-
Collected and cropped from J Cell Mol Med by CiteAb, provided under a CC-BY license
Image 1 of 7
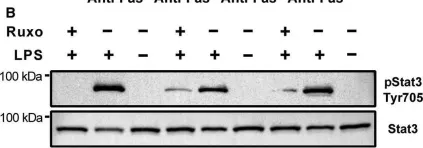
In J Cell Mol Med on 1 March 2020 by Markotic, A., Flegar, D., et al.
Fig.5.B

-
WB
-
Collected and cropped from J Cell Mol Med by CiteAb, provided under a CC-BY license
Image 1 of 7
In Cell Metab on 2 June 2015 by Varanita, T., Soriano, M. E., et al.
Fig.5.A

-
IHC
-
Collected and cropped from Cell Metab by CiteAb, provided under a CC-BY license
Image 1 of 7
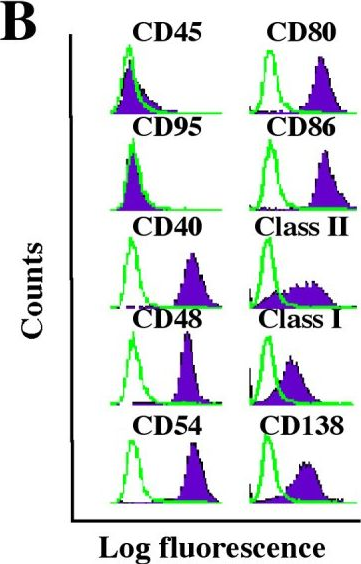
In Mol Immunol on 1 March 2009 by Shrimpton, R. E., Butler, M., et al.
Fig.4.A

-
FC/FACS
-
Collected and cropped from Mol Immunol by CiteAb, provided under a CC-BY license
Image 1 of 7
In Mol Immunol on 1 March 2009 by Shrimpton, R. E., Butler, M., et al.
Fig.4.B

-
FC/FACS
-
Collected and cropped from Mol Immunol by CiteAb, provided under a CC-BY license
Image 1 of 7
In Mol Cancer on 9 November 2005 by Han, S. S., Shaffer, A. L., et al.
Fig.1.B
-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Mol Cancer by CiteAb, provided under a CC-BY license
Image 1 of 7