Folic acid has been associated with fetal development, especially in fetal immunity. Therefore, limited evidence regarding the effects of different folic acid supplementation of hepatitis B surface antigen (HBsAg) positive mothers in innate immunity in offspring. Herein, this study aimed to explore the association between folic acid supplementation and the innate immunity of neonates and the immunological efficacy of hepatitis B vaccine (HepB), which may provide insights that could inform pre-pregnancy health management in HBsAg-positive mothers.
It is an ambispective cohort study with 293 pairs of HBsAg-positive mothers-offspring in Taiyuan, Shanxi Province, China. Mothers were classified into three groups according to the time of starting folic acid supplementation, non-supplementation group, pre-pregnancy group and post-pregnancy supplementation group. Immunological indexes such as immune cells proportion and innate immune mediators in cord blood and anti-HBs in infants were measured. Differences in immunological indexes were analyzed by One-Way ANOVA test. Univariate and multivariate analyses were performed for factors associated with abnormal immunological indexes and potential confounders were adjusted.
The preconception folic acid group showed a significantly higher expression levels of STING (P = 0.005) and pNF-κB (P = 0.010) in cord blood along with higher anti-HBs titres (P = 0.006), when compared to both non-supplementation group and post-pregnancy supplementation group. Higher anti-HBs levels indicate a stronger immune response to HepB and may enhance protection against HBV infection during early life. Infants in the high pNF-κB expression group exhibited a significantly elevated seropositive rate of HepB compared to those in the low pNF-κB expression group (P = 0.037). There were no mediation effects and no moderation effects in this study, potentially due to the direct influence of folic acid supplementation on immune responses or the limited sample size.
In conclusion, our findings demonstrate that preconception folic acid supplementation may enhance HepB vaccine responsiveness in infants of HBsAg-positive mothers. Meanwhile, high pNF-κB expression in cord blood can increase seropositive rates in infants. This discovery has significant public health implications, as it may provide a simple and accessible intervention to improve vaccination outcomes and reduce HBV transmission in endemic regions.
Copyright © 2025 Lian, Men, Xu, Li, Li, Wang, Yao, Li, Qu, Feng and Wang.
Product Citations: 321
In Frontiers in Nutrition on 8 May 2025 by Lian, J., Men, Z., et al.
-
Immunology and Microbiology
In IScience on 18 April 2025 by Liu, H., Ge, W., et al.
Hepatocellular carcinoma (HCC) resists immunotherapy due to its immunosuppressive microenvironment. Sarcoma homology 2 domain-containing protein tyrosine phosphatase-1 (SHP-1) inhibits T cell receptor signaling, and its pharmacological inhibition is limited by poor selectivity and membrane permeability. Here, we generated CRISPR-edited SHP-1-knockout (KO) CD8+ T cells to enhance adoptive therapy against HCC. Single-cell RNA sequencing of HCC patient T cells revealed elevated SHP-1 in exhausted subsets. SHP-1-KO T cells exhibited increased effector memory T cells (TEM) proportions and enhanced IFN-γ/Granzyme B/perforin secretion, improving cytotoxicity against HCC lines. In humanized PDX models, SHP-1-KO T cells demonstrated superior tumor-killing activity. Transcriptomics identified upregulated lipid metabolism pathways, with HMGCR as a hub gene. Combining SHP-1-KO T cells with simvastatin (HMGCR inhibitor) synergistically amplified anti-HCC efficacy. This study proposes a dual strategy combining SHP-1-targeted cell therapy and metabolic modulation to overcome immunotherapy resistance, offering a translatable approach for HCC treatment.
© 2025 The Author(s).
-
Cancer Research
In Drug Design, Development and Therapy on 3 March 2025 by Kong, X., Lin, Y., et al.
Human interleukin-2 (IL-2) stimulates the differentiation and expansion of diverse immune cells dose-dependently. As an immunotherapy agent to treat metastatic cancers, IL-2 has been used in clinical practice and has demonstrated clear antitumor effects; however, its short half-life, the risk of capillary leak syndrome, and the unintended activation of immunosuppressive Treg cells hinder its clinical application. To address these challenges, a novel PEGylated interleukin-2 analogue, SHR-1916, was designed. Its cellular selectivity, efficacy, and improved pharmacokinetic profiles were investigated.
The binding affinities were characterized by surface plasmon resonance (SPR) in vitro. Subsequently, the stimulatory properties were investigated in a murine cell line (CTLL-2), a human cell line (M07e), and human peripheral blood mononuclear cells (PBMCs). To assess the anti-tumor efficacy, a CT-26 colon carcinoma syngeneic model in BALB/c mice and a A375 human melanoma xenograft model using PBMC humanized NCG mice were used in vivo. Moreover, the pharmacokinetic behavior following a single intravenous or subcutaneous dose was evaluated in Sprague-Dawley rats.
SHR-1916 abolished binding to its receptor IL-2Rα, as evidenced by SPR assays, and exerted its activity mainly through binding to IL-2Rβγ, as confirmed by CTLL-2 and M07e cell proliferation assays. In contrast to IL-2, SHR-1916 exhibited a more biased activation of CD8+ T and NK cells compared to Treg cells and stimulated an increase in IFNγ secretion in PBMCs dose-dependently without triggering the release of other potential side effect-associated cytokines. In CT26 colon carcinoma and A375 melanoma models, SHR-1916 significantly reduced the tumor burden. Pharmacokinetic results showed that SHR-1916 had a significantly prolonged half-life in rats.
SHR-1916 exhibited excellent cellular selectivity, anti-tumor efficacies, and improved pharmacokinetics. It has the potential to serve as a novel immunotherapeutic agent designed to enhance IL-2's immune-stimulating activities and promote its tolerability while reducing the immunoregulatory function of Treg cells.
© 2025 Kong et al.
-
Cancer Research
-
Immunology and Microbiology
In Cell Reports Medicine on 18 February 2025 by Look, T., Sankowski, R., et al.
Chimeric antigen receptor (CAR) T cell therapy is a promising immunotherapy against cancer. Although there is a growing interest in other cell types, a comparison of CAR immune effector cells in challenging solid tumor contexts is lacking. Here, we compare mouse and human NKG2D-CAR-expressing T cells, natural killer (NK) cells, and macrophages against glioblastoma, the most aggressive primary brain tumor. In vitro we show that T cell cancer killing is CAR dependent, whereas intrinsic cytotoxicity overrules CAR dependence for NK cells, and CAR macrophages reduce glioma cells in co-culture assays. In orthotopic immunocompetent glioma mouse models, systemically administered CAR T cells demonstrate superior accumulation in the tumor, and each immune cell type induces distinct changes in the tumor microenvironment. An otherwise low therapeutic efficacy is significantly enhanced by co-expression of pro-inflammatory cytokines in all CAR immune effector cells, underscoring the necessity for multifaceted cell engineering strategies to overcome the immunosuppressive solid tumor microenvironment.
Copyright © 2025 The Authors. Published by Elsevier Inc. All rights reserved.
-
Cancer Research
In Biomolecules on 7 January 2025 by St Thomas, N., Christopher, B. N., et al.
Cutaneous T-cell lymphoma (CTCL) is a rare T-cell malignancy characterized by inflamed and painful rash-like skin lesions that may affect large portions of the body's surface. Patients experience recurrent infections due to a compromised skin barrier and generalized immunodeficiency resulting from a dominant Th2 immune phenotype of CTCL cells. Given the role of the unfolded protein response (UPR) in normal and malignant T-cell development, we investigated the impact of UPR-inducing drugs on the viability, transcriptional networks, and Th2 phenotype of CTCL. We found that CTCL cells were >5-fold more sensitive to the proteasome inhibitor bortezomib (Btz) and exhibited a distinct signaling and transcriptional response compared to normal CD4+ cells. The CTCL response was dominated by the induction of the HSP70 family member HSPA6 (HSP70B') and, to a lesser extent, HSPA5 (BiP/GRP78). To understand the significance of these two factors, we used a novel isoform selective small-molecule inhibitor of HSPA5/6 (JG-023). JG-023 induced pro-apoptotic UPR signaling and enhanced the cytotoxic effects of proteasome inhibitors and other UPR-inducing drugs in CTCL but not normal T cells. Interestingly, JG-023 also selectively suppressed the production of Th2 cytokines in CTCL and normal CD4+ T cells. Conditioned media (CM) from CTCL were immunosuppressive to normal T cells through an IL-10-dependent mechanism. This immunosuppression could be reversed by JG-023, other HSP70 inhibitors, Btz, and combinations of these UPR-targeted drugs. Our study points to the importance of the UPR in the pathology of CTCL and demonstrates the potential of proteasome and targeted HSPA5/6 inhibitors for therapy.
-
FC/FACS
-
Biochemistry and Molecular biology
-
Cancer Research
-
Immunology and Microbiology
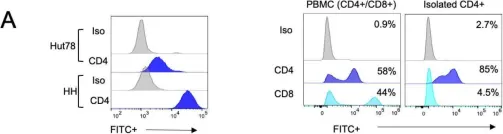
In Biomolecules on 7 January 2025 by St Thomas, N., Christopher, B. N., et al.
Fig.1.A

-
FC/FACS
-
Collected and cropped from Biomolecules by CiteAb, provided under a CC-BY license
Image 1 of 7
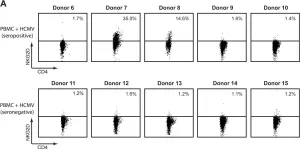
In Microbiol Spectr on 31 August 2022 by Castro Eiro, M. D., Natale, M. A., et al.
Fig.4.A

-
FC/FACS
-
Collected and cropped from Microbiol Spectr by CiteAb, provided under a CC-BY license
Image 1 of 7
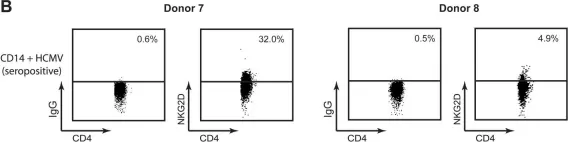
In Stem Cells Int on 2 August 2017 by Rubtsov, Y., Goryunov, К., et al.
Fig.4.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Stem Cells Int by CiteAb, provided under a CC-BY license
Image 1 of 7
In PLoS One on 8 August 2012 by Jensen, H., Folkersen, L., et al.
Fig.3.A

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 7
In PLoS One on 8 August 2012 by Jensen, H., Folkersen, L., et al.
Fig.3.B

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 7
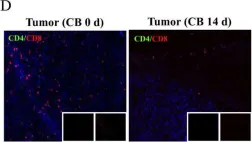
In BMC Cancer on 7 June 2011 by Lee, Y. S., Kim, T. S., et al.
Fig.1.C

-
FC/FACS
-
Collected and cropped from BMC Cancer by CiteAb, provided under a CC-BY license
Image 1 of 7
In BMC Cancer on 7 June 2011 by Lee, Y. S., Kim, T. S., et al.
Fig.1.D

-
IHC-IF
-
Collected and cropped from BMC Cancer by CiteAb, provided under a CC-BY license
Image 1 of 7