Antibody-dependent cell-mediated cytotoxic (ADCC) response mediated by natural killer (NK) cells correlates with decreased infection risk in studies involving simian immunodeficiency virus (SIV)/simian-human immunodeficiency virus (SHIV), and human immunodeficiency virus (HIV) vaccine candidates. Currently, the heterogeneities of the functional subset of rhesus macaque natural killer (RMNK) cells are under-characterized.
We engaged the RMNK cells with ADCC-mediating anti-HIV-1 monoclonal antibodies (ADCCAbs) or anti-CD16 antibodies and used CD107a expression as the surrogate marker for RMNK cells actively involved in ADCC. CD107a+ and CD107a- populations were analyzed individually using single-cell RNA sequencing.
Subsets of CD107a+ RMNK cells produced more chemokines than the others, suggesting that these cells not only eliminate infected cells but also provide immunoregulatory signals and potentially curb HIV-1 replication. Crosslinking of Fc gamma receptor IIIa via anti-CD16 antibodies resulted in a significantly higher percentage of degranulating cells than via ADCCAbs. However, the magnitude of degranulation and chemokine production was reduced by 6- to 30-fold.
The quality and quantity of receptor engagement are important determinants of achieving an optimal level of the RMNK response.
Copyright © 2025 Pathogens and Immunity.
Product Citations: 104
In Pathogens Immunity on 6 February 2025 by Nohara, J., Evangelous, T., et al.
-
FC/FACS
Preprint on BioRxiv : the Preprint Server for Biology on 27 September 2024 by Gurevic, I., Meudec, L., et al.
ABSTRACT Objective Our objective was to define the effect of JAK1/2 inhibitor (JAKinib) withdrawal on JAK/STAT biochemical response in the context of systemic rheumatic diseases. Methods We tested Type I (bind kinase active conformation) and Type II (bind kinase inactive conformation) JAKinibs in vitro using mesenchymal stromal cells and endothelial cells. We translated our findings in vivo studying NK cells from rheumatoid arthritis (RA) patients treated with Type I JAKinibs or methotrexate. Results Type I JAKinibs (ruxolitinib and baricitinib) increased phosphoJAK1 (pJAK1) and pJAK2 of IFNγ-stimulated MSCs and HUVECs in a time- and dose-dependent manner, with effect peaking after 24 hours. As expected, pSTAT1 was completely suppressed by JAKinibs. We found a marked and rapid increase of pSTATs upon discontinuation of Type I JAKinibs, that occurred to a lesser extent after Type II JAKinib withdrawal. Type I JAKinib withdrawal increased interferon and urokinase expression when compared to Type II JAKinib withdrawal. We found NK cells from RA patients taking Type I JAKinibs had a pro-inflammatory profile after JAKinib withdrawal compared to patients on methotrexate. Conclusions Type I JAKinibs paradoxically accumulate functionally defective pJAK. Upon withdrawal, the primed pJAKs are de-repressed and initiate a pSTAT signaling cascade, resulting in high interferon and urokinase. Type II JAKinibs do not cause pJAK accumulation, pSTAT cascade, and subsequent pro-inflammatory transcripts. The resultant cytokines and proteins produced from this cascade might be associated with adverse cardiac outcomes. Thus, JAKinib withdrawal is a possible mechanism contributing to the major adverse cardiac events described with JAKinib therapy.
-
Cardiovascular biology
In Nature Medicine on 1 March 2024 by Marin, D., Li, Y., et al.
There is a pressing need for allogeneic chimeric antigen receptor (CAR)-immune cell therapies that are safe, effective and affordable. We conducted a phase 1/2 trial of cord blood-derived natural killer (NK) cells expressing anti-CD19 chimeric antigen receptor and interleukin-15 (CAR19/IL-15) in 37 patients with CD19+ B cell malignancies. The primary objectives were safety and efficacy, defined as day 30 overall response (OR). Secondary objectives included day 100 response, progression-free survival, overall survival and CAR19/IL-15 NK cell persistence. No notable toxicities such as cytokine release syndrome, neurotoxicity or graft-versus-host disease were observed. The day 30 and day 100 OR rates were 48.6% for both. The 1-year overall survival and progression-free survival were 68% and 32%, respectively. Patients who achieved OR had higher levels and longer persistence of CAR-NK cells. Receiving CAR-NK cells from a cord blood unit (CBU) with nucleated red blood cells ≤ 8 × 107 and a collection-to-cryopreservation time ≤ 24 h was the most significant predictor for superior outcome. NK cells from these optimal CBUs were highly functional and enriched in effector-related genes. In contrast, NK cells from suboptimal CBUs had upregulation of inflammation, hypoxia and cellular stress programs. Finally, using multiple mouse models, we confirmed the superior antitumor activity of CAR/IL-15 NK cells from optimal CBUs in vivo. These findings uncover new features of CAR-NK cell biology and underscore the importance of donor selection for allogeneic cell therapies. ClinicalTrials.gov identifier: NCT03056339 .
© 2024. The Author(s).
-
Cancer Research
-
Immunology and Microbiology
In Communications Biology on 18 July 2023 by Ofori, E. A., Garcia-Senosiain, A., et al.
Blood phagocytes, such as neutrophils and monocytes, generate reactive oxygen species (ROS) as a part of host defense response against infections. We investigated the mechanism of Fcγ-Receptor (FcγR) mediated ROS production in these cells to understand how they contribute to anti-malarial immunity. Plasmodium falciparum merozoites opsonized with naturally occurring IgG triggered both intracellular and extracellular ROS generation in blood phagocytes, with neutrophils being the main contributors. Using specific inhibitors, we show that both FcγRIIIB and FcγRIIA acted synergistically to induce ROS production in neutrophils, and that NADPH oxidase 2 and the PI3K intracellular signal transduction pathway were involved in this process. High levels of neutrophil ROS were also associated with protection against febrile malaria in two geographically diverse malaria endemic regions from Ghana and India, stressing the importance of the cooperation between anti-malarial IgG and neutrophils in triggering ROS-mediated parasite killing as a mechanism for naturally acquired immunity against malaria.
© 2023. The Author(s).
-
Cardiovascular biology
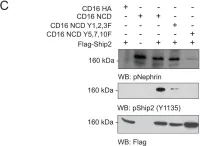
Rap1 Activity Is Essential for Focal Adhesion and Slit Diaphragm Integrity.
In Frontiers in Cell and Developmental Biology on 5 April 2022 by Maywald, M. L., Picciotto, C., et al.
Glomerular podocytes build, with their intercellular junctions, part of the kidney filter. The podocyte cell adhesion protein, nephrin, is essential for developing and maintaining slit diaphragms as functional loss in humans results in heavy proteinuria. Nephrin expression and function are also altered in many adult-onset glomerulopathies. Nephrin signals from the slit diaphragm to the actin cytoskeleton and integrin β1 at focal adhesions by recruiting Crk family proteins, which can interact with the Rap guanine nucleotide exchange factor 1 C3G. As Rap1 activity affects focal adhesion formation, we hypothesize that nephrin signals via Rap1 to integrin β. To address this issue, we combined Drosophila in vivo and mammalian cell culture experiments. We find that Rap1 is necessary for correct targeting of integrin β to focal adhesions in Drosophila nephrocytes, which also form slit diaphragm-like structures. In the fly, the Rap1 activity is important for signaling of the nephrin ortholog to integrin β, as well as for nephrin-dependent slit diaphragm integrity. We show by genetic interaction experiments that Rap1 functions downstream of nephrin signaling to integrin β and downstream of nephrin signaling necessary for slit diaphragm integrity. Similarly, in human podocyte culture, nephrin activation results in increased activation of Rap1. Thus, Rap1 is necessary for downstream signal transduction of nephrin to integrin β.
Copyright © 2022 Maywald, Picciotto, Lepa, Bertgen, Yousaf, Ricker, Klingauf, Krahn, Pavenstädt and George.
In PLoS One on 24 December 2011 by Venkatareddy, M., Cook, L., et al.
Fig.4.C

-
WB
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 1