Multiparameter tissue imaging enables analysis of cell-cell interactions in situ, the cellular basis for tissue structure, and novel cell types that are spatially restricted, giving clues to biological mechanisms behind tissue homeostasis and disease. Here, we streamlined and simplified the multiplexed imaging method CO-Detection by indEXing (CODEX) by validating 58 unique oligonucleotide barcodes that can be conjugated to antibodies. We showed that barcoded antibodies retained their specificity for staining cognate targets in human tissue. Antibodies were visualized one at a time by adding a fluorescently labeled oligonucleotide complementary to oligonucleotide barcode, imaging, stripping, and repeating this cycle. With this we developed a panel of 46 antibodies that was used to stain five human lymphoid tissues: three tonsils, a spleen, and a LN. To analyze the data produced, an image processing and analysis pipeline was developed that enabled single-cell analysis on the data, including unsupervised clustering, that revealed 31 cell types across all tissues. We compared cell-type compositions within and directly surrounding follicles from the different lymphoid organs and evaluated cell-cell density correlations. This sequential oligonucleotide exchange technique enables a facile imaging of tissues that leverages pre-existing imaging infrastructure to decrease the barriers to broad use of multiplexed imaging.
© 2021 The Authors. European Journal of Immunology published by Wiley-VCH GmbH.
Product Citations: 28
Highly multiplexed tissue imaging using repeated oligonucleotide exchange reaction.
In European Journal of Immunology on 1 May 2021 by Kennedy-Darling, J., Bhate, S. S., et al.
-
Immunology and Microbiology
In Scientific Reports on 11 March 2021 by Mishima, S., Kashiwakura, J. I., et al.
We previously reported that synovial mast cells (MCs) from patients with rheumatoid arthritis (RA) produced TNF-α in response to immune complexes via FcγRI and FcγRIIA. However, the specific functions of synovial MCs in RA remain unclear. This study aimed to elucidate those functions. Synovial tissues and fluid were obtained from RA and osteoarthritis (OA) patients undergoing joint replacement surgery. Synovium-derived, cultured MCs were generated by culturing dispersed synovial cells with stem cell factor. We performed microarray-based screening of mRNA and microRNA (miRNA), followed by quantitative RT-PCR-based verification. Synovial MCs from RA patients showed significantly higher prostaglandin systhetase (PTGS)1 and PTGS2 expression compared with OA patients' MCs, and they produced significantly more prostaglandin D2 (PGD2) following aggregation of FcγRI. PGD2 induced IL-8 production by human group 2 innate lymphoid cells, suggesting that PGD2-producing MCs induce neutrophil recruitment into the synovium of RA patients. PTGS2 mRNA expression in RA patients' MCs correlated inversely with miRNA-199a-3p expression, which down-regulated PTGS2. RA patients' synovial fluid contained significantly more PGD2 compared with OA patients' fluid. Synovial MCs might regulate inflammation in RA through hyper-production of PGD2 following FcRγ aggregation. Our findings indicate functional heterogeneity of human MCs among diseases.
In International Journal of Molecular Sciences on 21 March 2020 by Kim, J. H., Lim, I. R., et al.
Thymosin β4 (Tβ4) is a G-actin sequestering protein that contributes to diverse cellular activities, such as migration and angiogenesis. In this study, the beneficial effects of combined cell therapy with Tβ4 and human adipose-derived stem cells (hASCs) in a mouse ischemic hindlimb model were investigated. We observed that exogenous treatment with Tβ4 enhanced endogenous TMSB4X mRNA expression and promoted morphological changes (increased cell length) in hASCs. Interestingly, Tβ4 induced the active state of hASCs by up-regulating intracellular signaling pathways including the PI3K/AKT/mTOR and MAPK/ERK pathways. Treatment with Tβ4 significantly increased cell migration and sprouting from microbeads. Moreover, additional treatment with Tβ4 promoted the endothelial differentiation potential of hASCs by up-regulating various angiogenic genes. To evaluate the in vivo effects of the Tβ4-hASCs combination on vessel recruitment, dorsal window chambers were transplanted, and the co-treated mice were found to have a significantly increased number of microvessel branches. Transplantation of hASCs in combination with Tβ4 was found to improve blood flow and attenuate limb or foot loss post-ischemia compared to transplantation with hASCs alone. Taken together, the therapeutic application of hASCs combined with Tβ4 could be effective in enhancing endothelial differentiation and vascularization for treating hindlimb ischemia.
-
IF
-
Stem Cells and Developmental Biology
In Frontiers in Immunology on 2 April 2019 by Frumento, G., Zuo, J., et al.
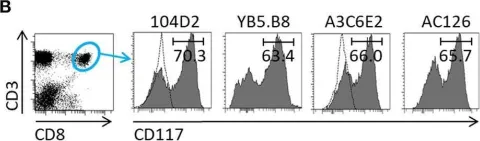
CD117 (cKit) is the receptor for stem cell factor (SCF) and plays an important role in early haemopoiesis. We show that CD117 is also expressed following priming of mature human CD8+ T cells in vitro and is detectable following primary infection in vivo. CD117 expression is mediated through an intrinsic pathway and is suppressed by IL-12. Importantly, the extent of CD117 expression is inversely related to the strength of the activating stimulus and subsequent engagement with cell-bound SCF markedly increases susceptibility to apoptosis. CD117 is therefore likely to shape the pattern of CD8+ T cell immunodominance during a primary immune response by rendering cells with low avidity for antigen more prone to apoptosis. Furthermore, CD117+ T cells are highly sensitive to apoptosis mediated by galectin-1, a molecule commonly expressed within the tumor microenvironment, and CD117 expression may therefore represent a novel and potentially targetable mechanism of tumor immune evasion.
-
FC/FACS
-
Immunology and Microbiology
In Frontiers in Oncology on 14 September 2018 by Bahmad, H. F., Cheaito, K., et al.
Cancer Stem Cells (CSCs) are a sub-population of cells, identified in most tumors, responsible for the initiation, recurrence, metastatic potential, and resistance of different malignancies. In prostate cancer (PCa), CSCs were identified and thought to be responsible for the generation of the lethal subtype, commonly known as Castration-Resistant Prostate Cancer (CRPC). In vitro models to investigate the properties of CSCs in PCa are highly required. Sphere-formation assay is an in vitro method commonly used to identify CSCs and study their properties. Here, we report the detailed methodology on how to generate and propagate spheres from PCa cell lines and from murine prostate tissue. This model is based on the ability of stem cells to grow in non-adherent serum-free gel matrix. We also describe how to use these spheres in histological and immuno-fluorescent staining assays to assess the differentiation potential of the CSCs. Our results show the sphere-formation Assay (SFA) as a reliable in vitro assay to assess the presence and self-renewal ability of CSCs in different PCa models. This platform presents a useful tool to evaluate the effect of conventional or novel agents on the initiation and self-renewing properties of different tumors. The effects can be directly evaluated through assessment of the sphere-forming efficiency (SFE) over five generations or other downstream assays such as immuno-histochemical analysis of the generated spheres.
-
Cancer Research
In Front Immunol on 2 April 2019 by Frumento, G., Zuo, J., et al.
Fig.1.B

-
FC/FACS
-
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 1