The relationship between chronic hepatitis B (CHB) infection and natural killer (NK) cell dysfunction is well-established, but the specific role of HBV viral antigens in driving NK cell impairment in patients with CHB remains unclear. This study investigates the modulatory effects of hepatitis B virus subviral particles (HBVsvp, a representative model for HBsAg) on the phenotypic regulation (activating and inhibitory receptors), cytokine production and cytotoxic potential of peripheral blood mononuclear cell-derived natural killer cells (PBMCs-derived NK cell), which contributes to NK cell dysfunction in CHB infection, potentially serving as an effective HBV immune evasion strategy by the virus.
NK cells were isolated from peripheral blood of patients with CHB (n=5) and healthy individuals (n=5), stimulated with HBVsvp. Subsequent flow cytometric characterization involved assessing changes in activating (NKp46 and NKG2D) and inhibitory (CD94) receptors expression, quantifying TNF-α and IFN- γ cytokine secretion, and evaluating the cytotoxic response against HepG2.2.15 cells with subsequent HBVsvp quantification.
In CHB patients, in vitro exposure of PBMCs-derived NK cell with HBVsvp (represent HBsAg model) significantly reduced NK cell-activating receptors expression (P = 0.022), increased expression of CD94 + NK cells (p = 0.029), accompanied with a reduced TNF-α - IFN-γ cytokine levels, and impaired cytotoxic capacity (evidenced by increased cell proliferation and elevated HBVsvp levels in co-cultures with HepG2.2.15 cells in a time-dependent), relative to healthy donors.
These findings suggest that HBVsvp may induce dysfunctional NK cell responses characterized by phenotypic imbalance with subsequent reduction in cytokine and cytotoxic levels, indicating HBVsvp immunosuppressive effect that compromises antiviral defense in CHB patients. These data enhance our understanding of NK cell interactions with HBsAg and highlight the potential for targeting CD94 inhibitory receptors to restore NK cell function as an immunotherapeutic approach. Further clinical research is needed to validate these observations and establish their utility as reliable biomarkers.
Copyright © 2024 Selim, Suef, Saied, Abdel-Maksoud, Almutairi, Aufy, Mousa, Mansour and Farag.
Product Citations: 14
In Frontiers in Immunology on 27 September 2024 by Selim, M. A., Suef, R. A., et al.
-
Homo sapiens (Human)
-
Immunology and Microbiology
CREB1 promotes expression of immune checkpoint HLA-E leading to immune escape in multiple myeloma.
In Leukemia on 1 August 2024 by Ismael, A., Robinette, A. J., et al.
Multiple myeloma (MM) cells effectively escape anti-tumoral immunity to survive in the tumor microenvironment (TME). Herein, we identify non-classical major histocompatibility complex (MHC) class I molecule HLA-E as a major contributing factor in immune escape. Clinically, HLA-E expression correlates with aggressive disease features such as t(4;14) and CD56 expression and is induced by IFN-gamma (IFN-γ) in the TME. We discovered that HLA-E is regulated by cAMP responsive element binding protein 1 (CREB1) transcription factor by direct promoter binding; genomic and pharmacological inhibition of CREB1 reduced HLA-E levels even in the presence of IFN-γ or IFN-γ activating agents, such as immunomodulatory drugs and panobinostat. HLA-E binds to natural killer group 2A (NKG2A), delivering an inhibitor signal to natural killer (NK) cells. Treatment with a CREB1 inhibitor was able to restore NK cell-mediated cytotoxicity against MM cell lines and patient samples. In conclusion, our results strongly demonstrate that CREB1 inhibition promotes anti-tumoral immunity in MM by limiting HLA-E expression and enhancing the activity of NK cells.
© 2024. The Author(s).
-
FC/FACS
-
Homo sapiens (Human)
-
Cancer Research
-
Immunology and Microbiology
In STAR Protocols on 15 December 2023 by Orta-Resendiz, A., Petitdemange, C., et al.
Here, we present a protocol for setting three spectral flow cytometry panels for the characterization of human unconventional CD8+NKG2A/C+ T cells as well as other T and natural killer cell subsets. We describe steps for standardizing, preparing, and staining the cells, the experimental setup, and the final data analysis. This protocol should be advantageous in various settings including immunophenotyping of limited samples, immune function evaluation/monitoring, as well as research in oncology, autoimmune, and infectious diseases.
Copyright © 2023 The Authors. Published by Elsevier Inc. All rights reserved.
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
Pro- and Anti-Inflammatory Cytokines in the Context of NK Cell-Trophoblast Interactions.
In International Journal of Molecular Sciences on 21 February 2022 by Mikhailova, V., Grebenkina, P., et al.
During pregnancy, uterine NK cells interact with trophoblast cells. In addition to contact interactions, uterine NK cells are influenced by cytokines, which are secreted by the cells of the decidua microenvironment. Cytokines can affect the phenotypic characteristics of NK cells and change their functional activity. An imbalance of pro- and anti-inflammatory signals can lead to the development of reproductive pathology. The aim of this study was to assess the effects of cytokines on NK cells in the presence of trophoblast cells in an in vitro model. We used TNFα, IFNγ, TGFβ and IL-10; the NK-92 cell line; and peripheral blood NK cells (pNKs) from healthy, non-pregnant women. For trophoblast cells, the JEG-3 cell line was used. In the monoculture of NK-92 cells, TNFα caused a decrease in CD56 expression. In the coculture of NK cells with JEG-3 cells, TNFα increased the expression of NKG2C and NKG2A by NK-92 cells. Under the influence of TGFβ, the expression of CD56 increased and the expression of NKp30 decreased in the monoculture. After the preliminary cultivation of NK-92 cells in the presence of TGFβ, their cytotoxicity increased. In the case of adding TGFβ to the PBMC culture, as well as coculturing PBMCs and JEG-3 cells, the expression of CD56 and NKp44 by pNK cells was reduced. The differences in the effects of TGFβ in the model using NK-92 cells and pNK cells may be associated with the possible influence of monocytes or other lymphoid cells from the mononuclear fraction.
-
Immunology and Microbiology
In Cell Stem Cell on 2 August 2018 by Li, Y., Hermanson, D. L., et al.
Chimeric antigen receptors (CARs) significantly enhance the anti-tumor activity of immune effector cells. Although most studies have evaluated CAR expression in T cells, here we evaluate different CAR constructs that improve natural killer (NK) cell-mediated killing. We identified a CAR containing the transmembrane domain of NKG2D, the 2B4 co-stimulatory domain, and the CD3ζ signaling domain to mediate strong antigen-specific NK cell signaling. NK cells derived from human iPSCs that express this CAR (NK-CAR-iPSC-NK cells) have a typical NK cell phenotype and demonstrate improved anti-tumor activity compared with T-CAR-expressing iPSC-derived NK cells (T-CAR-iPSC-NK cells) and non-CAR-expressing cells. In an ovarian cancer xenograft model, NK-CAR-iPSC-NK cells significantly inhibited tumor growth and prolonged survival compared with PB-NK cells, iPSC-NK cells, or T-CAR-iPSC-NK cells. Additionally, NK-CAR-iPSC-NK cells demonstrate in vivo activity similar to that of T-CAR-expressing T cells, although with less toxicity. These NK-CAR-iPSC-NK cells now provide standardized, targeted "off-the-shelf" lymphocytes for anti-cancer immunotherapy.
Copyright © 2018 Elsevier Inc. All rights reserved.
-
Cancer Research
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
In PLoS One on 8 August 2012 by Jensen, H., Folkersen, L., et al.
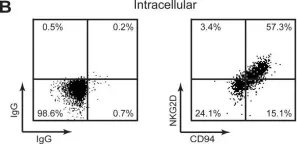
Fig.4.B

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 2
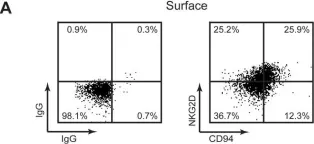
In PLoS One on 8 August 2012 by Jensen, H., Folkersen, L., et al.
Fig.4.A

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 2