Gastric cancer is primarily treated by surgery; however, little is known about the changes in the intraperitoneal immune environment and the prognostic impact of surgery. Surgical stress and cancer-associated inflammation cause immune cells to mobilize into the abdominal cavity via numerous cytokines. One such cytokine, CX3CR1, has various immune-related functions that remain to be fully explained. We characterized the intraperitoneal immune environment by investigating CX3CR1+ cells in intraperitoneal lavage fluid during gastric cancer surgery.
Lavage fluid samples were obtained from a total of 41 patients who underwent gastrectomy. The relative expression of various genes was analyzed using quantitative real-time PCR. The association of each gene expression with clinicopathological features and surgical outcomes was examined. The fraction of CX3CR1+ cells was analyzed by flow cytometry. Cytokine profiles in lavage fluid samples were investigated using a cytometric beads array.
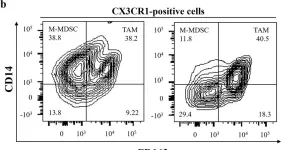
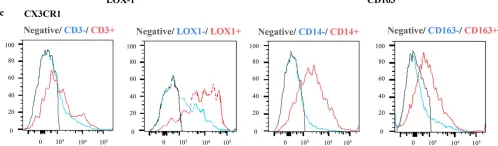
CX3CR1high patients exhibited higher levels of perioperative inflammation in blood tests and more recurrences than CX3CR1low patients. CX3CR1high patients tended to exhibit higher pathological T and N stage than CX3CR1low patients. CX3CR1 was primarily expressed on myeloid-derived suppressor cells and tumor-associated macrophages. In particular, polymorphonuclear myeloid-derived suppressor cells were associated with perioperative inflammation, pathological N, and recurrences. These immunosuppressive cells were associated with a trend toward unfavorable prognosis. Moreover, CX3CR1 expression was correlated with programmed death-1 expression.
Our results suggest that CX3CR1+ cells are associated with an acute inflammatory response, tumor-promotion, and recurrence. CX3CR1 expression could be taken advantage of as a beneficial therapeutic target for improving immunosuppressive state in the future. In addition, analysis of intra-abdominal CX3CR1+ cells could be useful for characterizing the immune environment after gastric cancer surgery.
© 2024. The Author(s).
Product Citations: 59
In World Journal of Surgical Oncology on 4 March 2024 by Natsuki, S., Yoshii, M., et al.
-
FC/FACS
-
Homo sapiens (Human)
-
Cancer Research
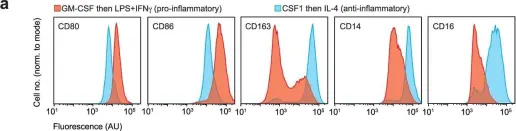
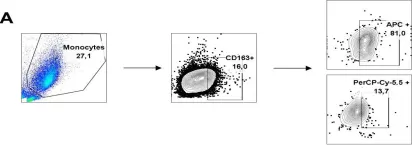
In Cell Reports Medicine on 20 February 2024 by Becker, A. M. D., Decker, A. H., et al.
The human dendritic cell (DC) family has recently been expanded by CD1c+CD14+CD163+ DCs, introduced as DC3s. DC3s are found in tumors and peripheral blood of cancer patients. Here, we report elevated frequencies of CD14+ cDC2s, which restore to normal frequencies after tumor resection, in non-small cell lung cancer patients. These CD14+ cDC2s phenotypically resemble DC3s and exhibit increased PD-L1, MERTK, IL-10, and IDO expression, consistent with inferior T cell activation ability compared with CD14- cDC2s. In melanoma patients undergoing CD1c+ DC vaccinations, increased CD1c+CD14+ DC frequencies correlate with reduced survival. We demonstrate conversion of CD5+/-CD1c+CD14- cDC2s to CD14+ cDC2s by tumor-associated factors, whereas monocytes failed to express CD1c under similar conditions. Targeted proteomics identified IL-6 and M-CSF as dominant drivers, and we show that IL-6R and CSF1R inhibition prevents tumor-induced CD14+ cDC2s. Together, this indicates cDC2s as direct pre-cursors of DC3-like CD1c+CD14+ DCs and provides insights into the importance and modulation of CD14+ DC3s in anti-tumor immune responses.
Copyright © 2024 The Authors. Published by Elsevier Inc. All rights reserved.
-
Homo sapiens (Human)
-
Cancer Research
-
Immunology and Microbiology
Preprint on Research Square on 6 December 2023 by Natsuki, S., Yoshii, M., et al.
Background: Gastric cancer is primarily treated by surgery; however, little is known about the changes in the intraperitoneal immune environment and the prognostic impact of surgery. Surgical stress and cancer-associated inflammation cause immune cells to mobilize into the abdominal cavity via numerous cytokines. One such cytokine, CX3CR1, has various immune-related functions that remain to be fully explained. We characterized the intraperitoneal immune environment by investigating CX3CR1 + cells in intraperitoneal lavage fluid during gastric cancer surgery. Methods Lavage fluid samples were obtained from a total of 41 patients who underwent gastrectomy. The relative expression of various genes was analyzed using quantitative real-time PCR. The association of each gene expression with clinicopathological features and surgical outcomes was examined. The fraction of CX3CR1 + cells was analyzed by flow cytometry. Cytokine profiles in lavage fluid samples were investigated using a cytometric beads array. Results CX3CR1 high patients exhibited higher levels of perioperative inflammation in blood tests and more recurrences than CX3CR1 low patients. CX3CR1 high patients tended to exhibit higher pathological T and N stage than CX3CR1 low patients. CX3CR1 was primarily expressed on myeloid-derived suppressor cells and tumor-associated macrophages. In particular, polymorphonuclear myeloid-derived suppressor cells were associated with perioperative inflammation, pathological N, and recurrences. These immunosuppressive cells were associated with a trend toward unfavorable prognosis. Moreover, CX3CR1 expression was correlated with programmed death–1 expression. Conclusions Our results suggest that CX3CR1 + cells are associated with an acute inflammatory response, tumor-promotion, and recurrence. CX3CR1 expression could be taken advantage of as a beneficial therapeutic target for improving immunosuppressive state in the future. In addition, analysis of intra-abdominal CX3CR1 + cells could be useful for characterizing the immune environment after gastric cancer surgery.
-
Homo sapiens (Human)
-
Cancer Research
In IScience on 17 November 2023 by Chen, G., Calcaterra, F., et al.
The C-C chemokine receptor type 5 (CCR5) expressed on immune cells supports inflammatory responses by directing cells to the inflammation site. CCR5 is also a major coreceptor for macrophage tropic human immunodeficiency viruses (R5-HIV-1) and its variants can confer protection from HIV infection, making it an ideal candidate to target for therapy. We developed a stepwise protocol that differentiates induced pluripotent stem cells (iPSCs) from individuals homozygous for the CCR5Δ32 variant and healthy volunteers into myeloid lineage induced monocytes (iMono) and macrophages (iMac). By characterizing iMono and iMac against their primary counterparts, we demonstrated that CCR5Δ32 homozygous cells are endowed with similar pluripotent potential for self-renewal and differentiation as iPSC lines generated from non-variant individuals while also showing resistance to HIV infection. In conclusion, these cells are a platform to investigate CCR5 pathophysiology in HIV-positive and negative individuals and to help develop novel therapies.
-
Stem Cells and Developmental Biology
In IScience on 21 July 2023 by Al-Rashed, F., Haddad, D., et al.
Foamy and inflammatory macrophages play pathogenic roles in metabolic disorders. However, the mechanisms that promote foamy and inflammatory macrophage phenotypes under acute-high-fat feeding (AHFF) remain elusive. Herein, we investigated the role of acyl-CoA synthetase-1 (ACSL1) in favoring the foamy/inflammatory phenotype of monocytes/macrophages upon short-term exposure to palmitate or AHFF. Palmitate exposure induced a foamy/inflammatory phenotype in macrophages which was associated with increased ACSL1 expression. Inhibition/knockdown of ACSL1 in macrophages suppressed the foamy/inflammatory phenotype through the inhibition of the CD36-FABP4-p38-PPARδ signaling axis. ACSL1 inhibition/knockdown suppressed macrophage foaming/inflammation after palmitate stimulation by downregulating the FABP4 expression. Similar results were obtained using primary human monocytes. As expected, oral administration of ACSL1 inhibitor triacsin-C in mice before AHFF normalized the inflammatory/foamy phenotype of the circulatory monocytes by suppressing FABP4 expression. Our results reveal that targeting ACSL1 leads to the attenuation of the CD36-FABP4-p38-PPARδ signaling axis, providing a therapeutic strategy to prevent the AHFF-induced macrophage foaming and inflammation.
© 2023 The Author(s).
-
Immunology and Microbiology
In World J Surg Oncol on 4 March 2024 by Natsuki, S., Yoshii, M., et al.
Fig.2.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from World J Surg Oncol by CiteAb, provided under a CC-BY license
Image 1 of 7
In World J Surg Oncol on 4 March 2024 by Natsuki, S., Yoshii, M., et al.
Fig.2.C

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from World J Surg Oncol by CiteAb, provided under a CC-BY license
Image 1 of 7
In World J Surg Oncol on 4 March 2024 by Natsuki, S., Yoshii, M., et al.
Fig.2.E

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from World J Surg Oncol by CiteAb, provided under a CC-BY license
Image 1 of 7
In Nature on 1 May 2023 by Solier, S., Müller, S., et al.
Fig.1.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nature by CiteAb, provided under a CC-BY license
Image 1 of 7
In PLoS Negl Trop Dis on 1 March 2017 by Silva, R. L., Santos, M. B., et al.
Fig.5.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from PLoS Negl Trop Dis by CiteAb, provided under a CC-BY license
Image 1 of 7
In PLoS Negl Trop Dis on 1 March 2017 by Silva, R. L., Santos, M. B., et al.
Fig.4.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from PLoS Negl Trop Dis by CiteAb, provided under a CC-BY license
Image 1 of 7
In PLoS Negl Trop Dis on 1 March 2017 by Silva, R. L., Santos, M. B., et al.
Fig.3.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from PLoS Negl Trop Dis by CiteAb, provided under a CC-BY license
Image 1 of 7