Allergic asthma has been linked to the activation of mast cells (MCs) by the neuropeptide substance P (SP), but the mechanism underlying this neuroimmune interaction is unknown. Substance P produced from cutaneous nociceptors activates MCs via Mas-related G-protein-coupled receptor B2 (MrgprB2) to enhance type 2 immune response in experimental atopic dermatitis in mice. We recently showed that the adapter protein β-arrestin2 (β-arr2) contributes to MrgprB2-mediated MC chemotaxis. The goals of this study were to determine if MrgprB2 facilitates neuroimmune interaction in IgE (FcεRI)-mediated allergic airway inflammation (AAI) and to assess if this response is modulated by β-arr2.
Wild-type (WT), MrgprB2-/- mice and mice with MC-specific deletion of β-arr2 (Cpa3Cre+ /β-arr2fl/fl ) were passively sensitized with anti-TNP-IgE and challenged with antigen. The generation of SP and MC recruitment in the lung were determined by immunofluorescence and toluidine blue staining, respectively. The transcripts for Tac1, MrgprB2, TNF-α, and Th2 cytokines in lung tissue were assessed by RT-PCR, and the release of selected cytokines in bronchoalveolar lavage (BAL) was determined by ELISA. Eosinophil and neutrophil recruitment in lung tissue and BAL were determined by immunofluorescence staining and flow cytometry, respectively. Goblet cell hyperplasia was determined by periodic acid-Schiff staining.
Following IgE sensitization and antigen challenge in WT mice, SP generation, and MC recruitment, transcripts for Tac1, MrgprB2, TNF-α, and Th2 cytokine were upregulated when compared to the control challenge. TNF-α, Th2 cytokine production, eosinophil/neutrophil recruitment, and goblet cell hyperplasia were also increased. These responses were significantly reduced in MrgprB2-/- and Cpa3Cre+ /β-arr2fl/fl mice.
The data presented herein suggest that SP-mediated MrgprB2 activation contributes to AAI and goblet cell hyperplasia in mice. Furthermore, these responses are modulated by β-arr2, which promotes MC recruitment to facilitate their activation through FcεRI.
Copyright © 2024 Sutradhar and Ali.
Product Citations: 41
In Frontiers in Immunology on 4 November 2024 by Sutradhar, S. & Ali, H.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
Allergic inflammation triggers dyslipidemia via IgG signalling.
In Allergy on 1 October 2024 by Fernández-Gallego, N., Castillo-González, R., et al.
Allergic diseases begin early in life and are often chronic, thus creating an inflammatory environment that may precede or exacerbate other pathologies. In this regard, allergy has been associated to metabolic disorders and with a higher risk of cardiovascular disease, but the underlying mechanisms remain incompletely understood.
We used a murine model of allergy and atherosclerosis, different diets and sensitization methods, and cell-depleting strategies to ascertain the contribution of acute and late phase inflammation to dyslipidemia. Untargeted lipidomic analyses were applied to define the lipid fingerprint of allergic inflammation at different phases of allergic pathology. Expression of genes related to lipid metabolism was assessed in liver and adipose tissue at different times post-allergen challenge. Also, changes in serum triglycerides (TGs) were evaluated in a group of 59 patients ≥14 days after the onset of an allergic reaction.
We found that allergic inflammation induces a unique lipid signature that is characterized by increased serum TGs and changes in the expression of genes related to lipid metabolism in liver and adipose tissue. Alterations in blood TGs following an allergic reaction are independent of T-cell-driven late phase inflammation. On the contrary, the IgG-mediated alternative pathway of anaphylaxis is sufficient to induce a TG increase and a unique lipid profile. Lastly, we demonstrated an increase in serum TGs in 59 patients after undergoing an allergic reaction.
Overall, this study reveals that IgG-mediated allergic inflammation regulates lipid metabolism.
© 2024 The Author(s). Allergy published by European Academy of Allergy and Clinical Immunology and John Wiley & Sons Ltd.
-
Immunology and Microbiology
Generation of nanobodies from transgenic 'LamaMice' lacking an endogenous immunoglobulin repertoire.
In Nature Communications on 3 June 2024 by Eden, T., Schaffrath, A. Z., et al.
Due to their exceptional solubility and stability, nanobodies have emerged as powerful building blocks for research tools and therapeutics. However, their generation in llamas is cumbersome and costly. Here, by inserting an engineered llama immunoglobulin heavy chain (IgH) locus into IgH-deficient mice, we generate a transgenic mouse line, which we refer to as 'LamaMouse'. We demonstrate that LamaMice solely express llama IgH molecules without association to Igκ or λ light chains. Immunization of LamaMice with AAV8, the receptor-binding domain of the SARS-CoV-2 spike protein, IgE, IgG2c, and CLEC9A enabled us to readily select respective target-specific nanobodies using classical hybridoma and phage display technologies, single B cell screening, and direct cloning of the nanobody-repertoire into a mammalian expression vector. Our work shows that the LamaMouse represents a flexible and broadly applicable platform for a facilitated selection of target-specific nanobodies.
© 2024. The Author(s).
NLRP3 inhibition attenuates the allergic rhinitis symptoms in an mice model
Preprint on Research Square on 27 September 2023 by Lee, M., Ko, Y., et al.
This study aimed to identify the mechanism underlying the activation of Nod-like receptor family, pyrin domain‐containing 3 (NLRP3) inflammasome signaling pathway in an ovalbumin (OVA)-induced allergic rhinitis (AR) mice model and to validate the effect of a specific inhibitor of the NLRP3, MCC950. Mice were divided into three groups and each group consisted of ten mice (saline group, the negative control group; OVA group, the OVA-induced AR model group; and OVA + MCC group, treated with 10 mg/kg MCC950). MCC950 was administered intraperitoneally every second day. Multiple parameters of AR, including NLRP3, caspase-1, interleukin (IL)-1β, and IL-18 were evaluated by using ELISA, RT-qPCR, histopathology, and immunohistochemistry. The mRNA and protein levels of NLRP3, caspase-1, IL-1β and IL-18 were upregulated in the OVA group compared with those of the saline group. MCC950 significantly inhibited the mRNA and protein levels of NLRP3, caspase-1, IL-1β and IL-18 in nasal tissue. Further, AR symptoms and eosinophil count were normalized after MCC950 treatment. However, OVA-specific IgE was not restored in the OVA + MCC group. In conclusion, NLRP3 inflammasome signaling pathway may be an alternative pathway to induce AR symptoms in OVA-induced AR model. MCC950 is a specific inhibitor of NLRP3 cascade, which attenuates AR symptoms regardless of IgE.
-
Mus musculus (House mouse)
Allergic inflammation triggers dyslipidemia via IgG signalling
Preprint on BioRxiv : the Preprint Server for Biology on 6 August 2023 by Fernández-Gallego, N., Castillo-González, R., et al.
ABSTRACT Background Allergic diseases begin early in life and are often chronic, thus creating an inflammatory environment that may precede or exacerbate other pathologies. In this regard, allergy has been associated to metabolic disorders and with a higher risk of cardiovascular disease, but the underlying mechanisms remain incompletely understood. Methods We used a murine model of allergy and atherosclerosis, different diets and sensitization methods, and cell-depleting strategies to ascertain the contribution of acute and late phase inflammation to dyslipidemia. Untargeted lipidomic analyses were applied to define the lipid fingerprint of allergic inflammation at different phases of allergic pathology. Expression of genes related to lipid metabolism was assessed in liver and adipose tissue at different times post-allergen challenge. Also, changes in serum triglycerides (TG) were evaluated in a group of 59 patients ≥14 days after the onset of an allergic reaction. Results We found that allergic inflammation induces a unique lipid signature that is characterized by increased serum TG and changes in the expression of genes related to lipid metabolism in liver and adipose tissue. Alterations in blood TGs following an allergic reaction are independent of T-cell-driven late phase inflammation. On the contrary, the IgG-mediated alternative pathway of anaphylaxis is sufficient to induce a TG increase and a unique lipid profile. Lastly, we demonstrated an increase in serum TG in 59 patients after undergoing an allergic reaction. Conclusion Overall, this study reveals that IgG-mediated allergic inflammation regulates lipid metabolism.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
In PLoS One on 10 November 2013 by Abramova, A., Sakaguchi, S., et al.
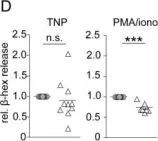
Fig.5.D

-
FC/FACS
-
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 1