T helper 17 (TH17) cells are implicated in autoimmune diseases, and several metabolic processes are shown to be important for their development and function. In this study, we report an essential role for sphingolipids synthesized through the de novo pathway in TH17 cell development. Deficiency of SPTLC1, a major subunit of serine palmitoyl transferase enzyme complex that catalyzes the first and rate-limiting step of de novo sphingolipid synthesis, impaired glycolysis in differentiating TH17 cells by increasing intracellular reactive oxygen species (ROS) through enhancement of nicotinamide adenine dinucleotide phosphate oxidase 2 activity. Increased ROS leads to impaired activation of mammalian target of rapamycin C1 and reduced expression of hypoxia-inducible factor 1-alpha and c-Myc-induced glycolytic genes. SPTLCI deficiency protected mice from developing experimental autoimmune encephalomyelitis and experimental T cell transfer colitis. Our results thus show a critical role for de novo sphingolipid biosynthetic pathway in shaping adaptive immune responses with implications in autoimmune diseases.
Product Citations: 16
Sphingolipid biosynthesis is essential for metabolic rewiring during TH17 cell differentiation.
In Science Advances on 26 April 2024 by Abimannan, T., Parthibane, V., et al.
-
FC/FACS
-
Biochemistry and Molecular biology
-
Cell Biology
Tumor immunogenicity dictates reliance on TCF1 in CD8+ T cells for response to immunotherapy.
In Cancer Cell on 11 September 2023 by Escobar, G., Tooley, K., et al.
Stem-like CD8+ T cells are regulated by T cell factor 1 (TCF1) and are considered requisite for immune checkpoint blockade (ICB) response. However, recent findings indicate that reliance on TCF1+CD8+ T cells for ICB efficacy may differ across tumor contexts. We find that TCF1 is essential for optimal priming of tumor antigen-specific CD8+ T cells and ICB response in poorly immunogenic tumors that accumulate TOX+ dysfunctional T cells, but is dispensable for T cell priming and therapy response in highly immunogenic tumors that efficiently expand transitory effectors. Importantly, improving T cell priming by vaccination or by enhancing antigen presentation on tumors rescues the defective responses of TCF1-deficient CD8+ T cells upon ICB in poorly immunogenic tumors. Our study highlights TCF1's role during the early stages of anti-tumor CD8+ T cell responses with important implications for guiding optimal therapeutic interventions in cancers with low TCF1+CD8+ T cells and low-neo-antigen expression.
Copyright © 2023 Elsevier Inc. All rights reserved.
-
Cancer Research
-
Immunology and Microbiology
SREBP signaling is essential for effective B cell responses.
In Nature Immunology on 1 February 2023 by Luo, W., Adamska, J. Z., et al.
Our previous study using systems vaccinology identified an association between the sterol regulatory binding protein (SREBP) pathway and humoral immune response to vaccination in humans. To investigate the role of SREBP signaling in modulating immune responses, we generated mice with B cell- or CD11c+ antigen-presenting cell (APC)-specific deletion of SCAP, an essential regulator of SREBP signaling. Ablation of SCAP in CD11c+ APCs had no effect on immune responses. In contrast, SREBP signaling in B cells was critical for antibody responses, as well as the generation of germinal centers,memory B cells and bone marrow plasma cells. SREBP signaling was required for metabolic reprogramming in activated B cells. Upon mitogen stimulation, SCAP-deficient B cells could not proliferate and had decreased lipid rafts. Deletion of SCAP in germinal center B cells using AID-Cre decreased lipid raft content and cell cycle progression. These studies provide mechanistic insights coupling sterol metabolism with the quality and longevity of humoral immunity.
© 2022. The Author(s), under exclusive licence to Springer Nature America, Inc.
-
Immunology and Microbiology
In The Journal of Immunology on 1 April 2022 by Wemlinger, S. M., Parker Harp, C. R., et al.
The BCR comprises a membrane-bound Ig that is noncovalently associated with a heterodimer of CD79A and CD79B. While the BCR Ig component functions to sense extracellular Ag, CD79 subunits contain cytoplasmic ITAMs that mediate intracellular propagation of BCR signals critical for B cell development, survival, and Ag-induced activation. CD79 is therefore an attractive target for Ab and chimeric Ag receptor T cell therapies for autoimmunity and B cell neoplasia. Although the mouse is an attractive model for preclinical testing, due to its well-defined immune system, an obstacle is the lack of cross-reactivity of candidate therapeutic anti-human mAbs with mouse CD79. To overcome this problem, we generated knockin mice in which the extracellular Ig-like domains of CD79A and CD79B were replaced with human equivalents. In this study, we describe the generation and characterization of mice expressing chimeric CD79 and report studies that demonstrate their utility in preclinical analysis of anti-human CD79 therapy. We demonstrate that human and mouse CD79 extracellular domains are functionally interchangeable, and that anti-human CD79 lacking Fc region effector function does not cause significant B cell depletion, but induces 1) decreased expression of plasma membrane-associated IgM and IgD, 2) uncoupling of BCR-induced tyrosine phosphorylation and calcium mobilization, and 3) increased expression of PTEN, consistent with the levels observed in anergic B cells. Finally, anti-human CD79 treatment prevents disease development in two mouse models of autoimmunity. We also present evidence that anti-human CD79 treatment may inhibit Ab secretion by terminally differentiated plasmablasts and plasma cells in vitro.Copyright © 2022 by The American Association of Immunologists, Inc.
-
Immunology and Microbiology
HLA-independent T cell receptors for targeting tumors with low antigen density.
In Nature Medicine on 1 February 2022 by Mansilla-Soto, J., Eyquem, J., et al.
Chimeric antigen receptors (CARs) are receptors for antigen that direct potent immune responses. Tumor escape associated with low target antigen expression is emerging as one potential limitation of their efficacy. Here we edit the TRAC locus in human peripheral blood T cells to engage cell-surface targets through their T cell receptor-CD3 complex reconfigured to utilize the same immunoglobulin heavy and light chains as a matched CAR. We demonstrate that these HLA-independent T cell receptors (HIT receptors) consistently afford high antigen sensitivity and mediate tumor recognition beyond what CD28-based CARs, the most sensitive design to date, can provide. We demonstrate that the functional persistence of HIT T cells can be augmented by constitutive coexpression of CD80 and 4-1BBL. Finally, we validate the increased antigen sensitivity afforded by HIT receptors in xenograft mouse models of B cell leukemia and acute myeloid leukemia, targeting CD19 and CD70, respectively. Overall, HIT receptors are well suited for targeting cell surface antigens of low abundance.
© 2022. The Author(s), under exclusive licence to Springer Nature America, Inc.
-
Cancer Research
-
Immunology and Microbiology
In PLoS One on 11 August 2011 by Deswal, S., Schulze, A. K., et al.
Fig.3.B
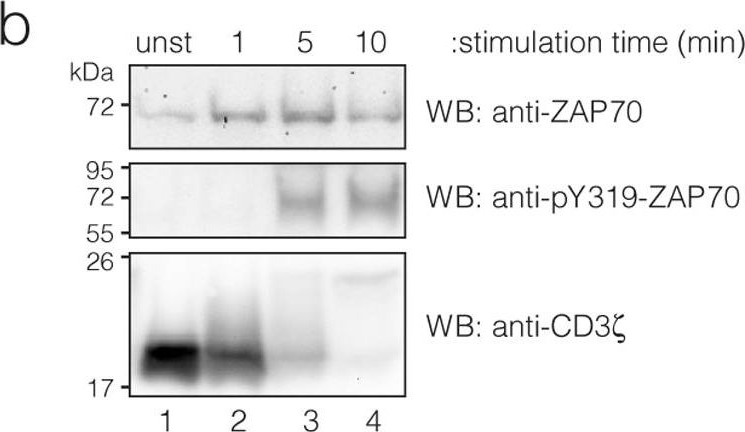
-
WB
-
Mus musculus (House mouse)
Collected and cropped from PLoS ONE by CiteAb, provided under a CC-BY license
Image 1 of 2
In PLoS One on 11 August 2011 by Deswal, S., Schulze, A. K., et al.
Fig.1.D
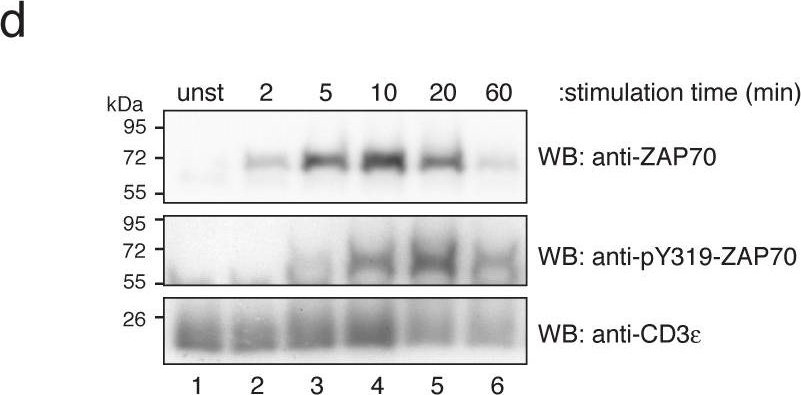
-
WB
-
Mus musculus (House mouse)
Collected and cropped from PLoS ONE by CiteAb, provided under a CC-BY license
Image 1 of 2