The effector function of T cells is regulated via immune checkpoints, activating or inhibiting the immune response. The BTLA-HVEM complex, the inhibitory immune checkpoint, may act as one of the tumor immune escape mechanisms. Therefore, interfering with the binding of these proteins can prove beneficial in cancer treatment. Our study focused on peptides interacting with HVEM at the same place as BTLA, thus disrupting the BTLA-HVEM interaction. These peptides' structure and amino acid sequences are based on the gD protein, the ligand of HVEM. Here, we investigated their immunomodulatory potential in melanoma patients.
Flow cytometry analyses of activation, proliferation, and apoptosis of T cells from patients were performed. Additionally, we evaluated changes within the T cell memory compartment.
The most promising compound - Pep(2), increased the percentages of activated T cells and promoted their proliferation. Additionally, this peptide affected the proliferation rate and apoptosis of melanoma cell line in co-culture with T cells.
We conclude that the examined peptide may act as a booster for the immune system. Moreover, the adjuvant and activating properties of the gD-derived peptide could be used in a combinatory therapy with currently used ICI-based treatment. Our studies also demonstrate that even slight differences in the amino acid sequence of peptides and any changes in the position of the disulfide bond can strongly affect the immunomodulatory properties of compounds.
Copyright © 2024 Wojciechowicz, Kuncewicz, Rutkowski, Jassem, Wardowska and Spodzieja.
Product Citations: 7
In Frontiers in Immunology on 5 June 2024 by Wojciechowicz, K., Kuncewicz, K., et al.
-
Homo sapiens (Human)
-
Cancer Research
-
Immunology and Microbiology
In Nature Medicine on 1 March 2023 by Cascone, T., Leung, C. H., et al.
Neoadjuvant ipilimumab + nivolumab (Ipi+Nivo) and nivolumab + chemotherapy (Nivo+CT) induce greater pathologic response rates than CT alone in patients with operable non-small cell lung cancer (NSCLC). The impact of adding ipilimumab to neoadjuvant Nivo+CT is unknown. Here we report the results and correlates of two arms of the phase 2 platform NEOSTAR trial testing neoadjuvant Nivo+CT and Ipi+Nivo+CT with major pathologic response (MPR) as the primary endpoint. MPR rates were 32.1% (7/22, 80% confidence interval (CI) 18.7-43.1%) in the Nivo+CT arm and 50% (11/22, 80% CI 34.6-61.1%) in the Ipi+Nivo+CT arm; the primary endpoint was met in both arms. In patients without known tumor EGFR/ALK alterations, MPR rates were 41.2% (7/17) and 62.5% (10/16) in the Nivo+CT and Ipi+Nivo+CT groups, respectively. No new safety signals were observed in either arm. Single-cell sequencing and multi-platform immune profiling (exploratory endpoints) underscored immune cell populations and phenotypes, including effector memory CD8+ T, B and myeloid cells and markers of tertiary lymphoid structures, that were preferentially increased in the Ipi+Nivo+CT cohort. Baseline fecal microbiota in patients with MPR were enriched with beneficial taxa, such as Akkermansia, and displayed reduced abundance of pro-inflammatory and pathogenic microbes. Neoadjuvant Ipi+Nivo+CT enhances pathologic responses and warrants further study in operable NSCLC. (ClinicalTrials.gov registration: NCT03158129 .).
© 2023. The Author(s).
-
FC/FACS
-
Cancer Research
In Oncoimmunology on 8 November 2020 by Maas, R. J. A., Hoogstad-van Evert, J., et al.
Advanced ovarian cancer (OC) patients have a poor 5-year survival of only 28%, emphasizing the medical need for improved therapies. Adjuvant immunotherapy could be an attractive approach since OC is an immunogenic disease and the presence of tumor-infiltrating lymphocytes has shown to positively correlate with patient survival. Among these infiltrating lymphocytes are natural killer (NK) cells, key players involved in tumor targeting, initiated by signaling via activating and inhibitory receptors. Here, we investigated the role of the DNAM-1/TIGIT/CD96 axis in the anti-tumor response of NK cells toward OC. Ascites-derived NK cells from advanced OC patients showed lower expression of activating receptor DNAM-1 compared to healthy donor peripheral blood NK cells, while inhibitory receptor TIGIT and CD96 expression was equal or higher, respectively. This shift to a more inhibitory phenotype could also be induced in vitro by co-culturing healthy donor NK cells with OC tumor spheroids, and in vivo on intraperitoneally infused NK cells in SKOV-3 OC bearing NOD/SCID-IL2Rγnull (NSG) mice. Interestingly, TIGIT blockade enhanced degranulation and interferon gamma (IFNγ) production of healthy donor CD56dim NK cells in response to OC tumor cells, especially when DNAM-1/CD155 interactions were in place. Importantly, TIGIT blockade boosted functional responsiveness of CD56dim NK cells of OC patients with a baseline reactivity against SKOV-3 cells. Overall, our data show for the first time that checkpoint molecules TIGIT/DNAM-1/CD96 play an important role in NK cell responsiveness against OC, and provides rationale for incorporating TIGIT interference in NK cell-based immunotherapy in OC patients.
© 2020 The Author(s). Published with license by Taylor & Francis Group, LLC.
-
FC/FACS
-
Cancer Research
In Frontiers in Immunology on 17 April 2020 by Zhang, J. A., Lu, Y. B., et al.
Little is known about how tuberculosis (TB) impairs dendritic cell (DC) function and anti-TB immune responses. We previously showed that the B and T lymphocyte attenuator (BTLA), an immune inhibitory receptor, is involved in TB pathogenesis. Here, we examined whether BTLA expression in TB affects phenotypic and functional aspects of DCs. Active TB patients exhibited higher expression of BTLA in myeloid dendritic cells (mDCs) and plasmacytoid DCs (pDCs) subsets compared with healthy controls (HCs). BTLA expression was similarly high in untreated TB, TB relapse, and sputum-bacillus positive TB, but anti-TB therapy reduced TB-driven increases in frequencies of BTLA+ DCs. BTLA+ DCs in active TB showed decreased expression of the DC maturation marker CD83, with an increased expression of CCR7 in mDCs. BTLA+ DCs in active TB displayed a decreased ability to express HLA-DR and to uptake foreign antigen, with a reduced expression of the co-stimulatory molecule CD80, but not CD86. Functionally, BTLA+ DCs in active TB showed a decreased production of IL-12 and IFN-α as well as a reduced ability to stimulate allogeneic T-cell proliferative responses. BTLA+ mDCs produced larger amounts of IL-4 and TGF-β than BTLA- mDCs in both HCs and APT patients. BTLA+ DCs from active TB patients showed a reduced ability to stimulate Mtb antigen-driven Th17 and Th22 polarizations as compared to those from HCs. Conversely, these BTLA+ DCs more readily promoted the differentiation of T regulatory cells (Treg) and Th2 than those from HCs. These findings suggest that TB-driven BTLA expression in DCs impairs the expression of functional DC surrogate markers and suppress the ability of DCs to induce anti-TB Th17 and Th22 response while promoting Th2 and Foxp3+ Tregs.
Copyright © 2020 Zhang, Lu, Wang, Liu, Chen, Shen, Luo, Xu, Peng, Luo, Huang, Wu, Zheng, Yi, Chen and Xu.
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
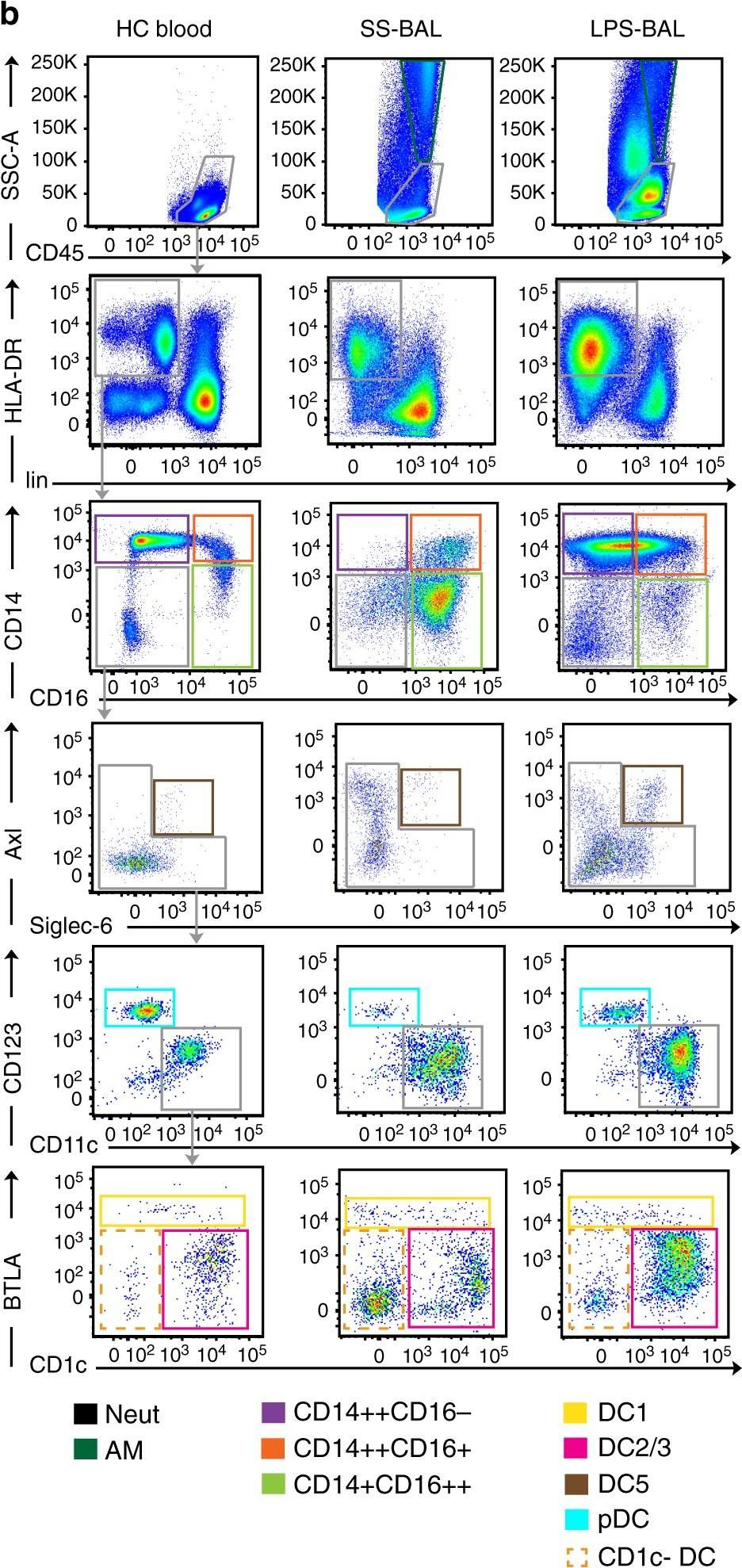
In Nature Communications on 30 April 2019 by Jardine, L., Wiscombe, S., et al.
Mononuclear phagocytes (MPs) including monocytes, macrophages and dendritic cells (DCs) are critical innate immune effectors and initiators of the adaptive immune response. MPs are present in the alveolar airspace at steady state, however little is known about DC recruitment in acute pulmonary inflammation. Here we use lipopolysaccharide inhalation to induce acute inflammation in healthy volunteers and examine the impact on bronchoalveolar lavage fluid and blood MP repertoire. Classical monocytes and two DC subsets (DC2/3 and DC5) are expanded in bronchoalveolar lavage fluid 8 h after lipopolysaccharide inhalation. Surface phenotyping, gene expression profiling and parallel analysis of blood indicate recruited DCs are blood-derived. Recruited monocytes and DCs rapidly adopt typical airspace-resident MP gene expression profiles. Following lipopolysaccharide inhalation, alveolar macrophages strongly up-regulate cytokines for MP recruitment. Our study defines the characteristics of human DCs and monocytes recruited into bronchoalveolar space immediately following localised acute inflammatory stimulus in vivo.
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
In Nat Commun on 30 April 2019 by Jardine, L., Wiscombe, S., et al.
Fig.3.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 3
In Nat Commun on 30 April 2019 by Jardine, L., Wiscombe, S., et al.
Fig.4.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 3
In Nat Commun on 30 April 2019 by Jardine, L., Wiscombe, S., et al.
Fig.1.B
-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 3


