Dysregulation of T follicular helper (Tfh) and T follicular regulatory (Tfr) cell homeostasis in germinal centers (GCs) can lead to antibody-mediated autoimmunity. While interleukin-1β (IL-1β) modulates the GC response via IL-1R1 and IL-1R2 receptors on follicular T cells in animal models, its role in humans remains unclear. We analyzed Tfh and Tfr phenotypes in human secondary lymphoid organs (tonsils, spleen, and mesenteric lymph nodes) using flow cytometry, single-cell transcriptomics, and in vitro culture, comparing findings with samples from autoimmune patients. We observed organ-specific Tfh/Tfr phenotypes according to activation status and IL-1 receptor expression. An excess of IL-1R1 over IL-1R2 expression promoted a unique activated Tfr subset with Treg and GC-Tfh features. IL-1β signaling via IL-1R1 enhanced follicular T-cell activation and Tfh-to-Tfr differentiation, while IL-1β inhibition upregulated IL-1R1, indicating a tightly regulated process. In autoimmune patients, high IL-1β and circulating Tfr levels correlated with increased autoantibody production, linking inflammation, IL-1β signaling, and Tfr/Tfh balance. Our findings highlight the critical role of IL-1β in follicular T-cell activation and suggest that targeting IL-1β signaling in Tfh and Tfr cells could be a promising strategy for treating antibody-mediated autoimmune diseases.
Product Citations: 38
IL-1β Signaling modulates T follicular helper and regulatory cells in human lymphoid tissues.
In JCI Insight on 20 May 2025 by Vaineau, R., Jeger-Madiot, R., et al.
In Cell Reports Medicine on 15 October 2024 by Wu, J., Bloch, N., et al.
The clinical use of interleukin-2 (IL-2) for cancer immunotherapy is limited by severe toxicity. Emerging IL-2 therapies with reduced IL-2 receptor alpha (IL-2Rα) binding aim to mitigate toxicity and regulatory T cell (Treg) expansion but have had limited clinical success. Here, we show that IL-2Rα engagement is critical for the anti-tumor activity of systemic IL-2 therapy. A "non-α" IL-2 mutein induces systemic expansion of CD8+ T cells and natural killer (NK) cells over Tregs but exhibits limited anti-tumor efficacy. We develop a programmed cell death protein 1 (PD-1)-targeted, receptor-masked IL-2 immunocytokine, PD1-IL2Ra-IL2, which attenuates systemic IL-2 activity while maintaining the capacity to engage IL-2Rα on PD-1+ T cells. Mice treated with PD1-IL2Ra-IL2 show no systemic toxicities observed with unmasked IL-2 treatment yet achieve robust tumor growth control. Furthermore, PD1-IL2Ra-IL2 can be effectively combined with other T cell-mediated immunotherapies to enhance anti-tumor responses. These findings highlight the therapeutic potential of PD1-IL2Ra-IL2 as a targeted, receptor-masked, and "α-maintained" IL-2 therapy for cancer.
Copyright © 2024 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Cancer Research
-
Immunology and Microbiology
In NPJ Precision Oncology on 20 May 2024 by Hermansen, J. U., Yin, Y., et al.
The microenvironment of hematologic cancers contributes to tumor cell survival and proliferation, as well as treatment resistance. Understanding tumor- and drug-induced changes to the immune cell composition and functionality is therefore critical for implementing optimal treatment strategies and for the development of novel cancer therapies. The liquid nature of peripheral blood makes this organ uniquely suited for single-cell studies by flow cytometry. (Phospho)protein profiles detected by flow cytometry analyses have been shown to correlate with ex vivo drug sensitivity and to predict treatment outcomes in hematologic cancers, demonstrating that this method is suitable for pre-clinical studies. Here, we present a flow cytometry protocol that combines multi-parameter immunophenotyping with single-cell (phospho)protein profiling. The protocol makes use of fluorescent cell barcoding, which means that multiple cell samples, either collected from different donors or exposed to different treatment conditions, can be combined and analyzed as one experiment. This reduces variability between samples, increases the throughput of the experiment, and lowers experimental costs. This protocol may serve as a guide for the use and further development of assays to study immunophenotype and cell signaling at single-cell resolution in normal and malignant cells. The read-outs may provide biological insight into cancer pathogenesis, identify novel drug targets, and ultimately serve as a biomarker to guide clinical decision-making.
© 2024. The Author(s).
-
Homo sapiens (Human)
Human inherited CCR2 deficiency underlies progressive polycystic lung disease.
In Cell on 18 January 2024 by Neehus, A. L., Carey, B., et al.
We describe a human lung disease caused by autosomal recessive, complete deficiency of the monocyte chemokine receptor C-C motif chemokine receptor 2 (CCR2). Nine children from five independent kindreds have pulmonary alveolar proteinosis (PAP), progressive polycystic lung disease, and recurrent infections, including bacillus Calmette Guérin (BCG) disease. The CCR2 variants are homozygous in six patients and compound heterozygous in three, and all are loss-of-expression and loss-of-function. They abolish CCR2-agonist chemokine C-C motif ligand 2 (CCL-2)-stimulated Ca2+ signaling in and migration of monocytic cells. All patients have high blood CCL-2 levels, providing a diagnostic test for screening children with unexplained lung or mycobacterial disease. Blood myeloid and lymphoid subsets and interferon (IFN)-γ- and granulocyte-macrophage colony-stimulating factor (GM-CSF)-mediated immunity are unaffected. CCR2-deficient monocytes and alveolar macrophage-like cells have normal gene expression profiles and functions. By contrast, alveolar macrophage counts are about half. Human complete CCR2 deficiency is a genetic etiology of PAP, polycystic lung disease, and recurrent infections caused by impaired CCL2-dependent monocyte migration to the lungs and infected tissues.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
-
FC/FACS
-
Homo sapiens (Human)
In American Journal of Reproductive Immunology (New York, N.Y. : 1989) on 1 January 2022 by Fernández, L., Grasso, E., et al.
Decidualized cells display an active role during embryo implantation sensing blastocyst quality, allowing the implantation of normal developed blastocysts and preventing the invasion of impaired developed ones. Here, we characterized the immune microenvironment generated by decidualized cells in response to soluble factors secreted by blastocysts that shape the receptive milieu.
We used an in vitro model of decidualization based on the Human Endometrial Stromal Cells line (HESC) differentiated with medroxiprogesterone and dibutyryl-cAMP, then treated with human blastocysts-conditioned media (BCM) classified according to their quality.
Decidualized cells treated with BCM from impaired developed blastocysts increased IL-1β production. Next, we evaluated the ability of decidualized cells to modulate other mediators associated with menstruation as chemokines. Decidualized cells responded to stimulation with BCM from impaired developed blastocysts increasing CXCL12 expression and CXCL8 secretion. The modulation of these markers was associated with the recruitment and activation of neutrophils, while regulatory T cells recruitment was restrained. These changes were not observed in the presence of BCM from normal developed blastocysts.
Soluble factors released by impaired developed blastocysts induce an exacerbated inflammatory response associated with neutrophils recruitment and activation, providing new clues to understand the molecular basis of the embryo-endometrial dialogue.
© 2021 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd.
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
In Mol Oncol on 1 April 2019 by Zhou, Z., Chen, H., et al.
Fig.6.C

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Mol Oncol by CiteAb, provided under a CC-BY license
Image 1 of 3
In Mol Oncol on 1 April 2019 by Zhou, Z., Chen, H., et al.
Fig.6.D

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Mol Oncol by CiteAb, provided under a CC-BY license
Image 1 of 3
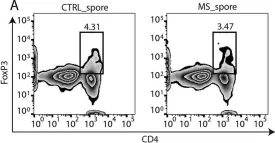
In mSystems on 13 November 2018 by Cekanaviciute, E., Pröbstel, A. K., et al.
Fig.2.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from mSystems by CiteAb, provided under a CC-BY license
Image 1 of 3