Several chronic inflammatory diseases have been linked to high-salt (HS) diets. Chronic inflammation is an established causative hallmark of cancer. However, a direct role of HS diets in tumorigenesis is yet to be defined. Previous orthotopic murine breast tumor studies have shown that short-term HS diets caused inhibition of tumor growth through the activation of cytotoxic adaptive immune responses. However, there have been experimental challenges in developing a viable chronic HS-diet-based murine tumor model. To address this, we have developed a novel chronic HS diet tumor model through the sequential passaging of tumor cells in mice under HS dietary conditions. Two orthotopic murine triple-negative breast cancer models, 4T1 tumor cells injected into BALB/c mice and Py230 tumor cells injected into C57Bl/6 mice, were utilized in our study. For the HS diet cohort, prior to orthotopic injection with tumor cells, the mice were kept on a 4% NaCl diet for 2 weeks. For the regular salt (RS) diet cohort, the mice were kept on a 1% NaCl diet. Following syngeneic cancer cell injection, tumors were allowed to grow for 28 days, following which they were collected to isolate immune cell-depleted cancer cells (passage 1, P1). The tumor cells from P1 were reinjected into the next set of non-tumor-bearing mice. This procedure was repeated for three cycles (P2-P4). In P1, compared to the RS diet cohort, we observed reduced tumor kinetics in both murine tumor models on the HS diet. In contrast, by P4, there was significantly higher tumor progression in the HS diet cohort over the RS diet cohort. Flow cytometry analysis demonstrated an 8-fold increase in tumor-initiating stem cells (TISCs) from P1 to P4 of the HS diet cohort, while there were no significant change in TISC frequency with sequential passaging in the RS diet cohort. Molecular studies showed enhanced expression of TGFβR2 and CD80 on TISCs isolated from the P4 HS diet cohort. In vitro studies demonstrated that TGFβ stimulation of these TISCs increased the cellular expression of CD80 molecules. Further, the chronic HS diet selectively induced the glycolytic metabolic phenotype over the mitochondrial oxidative phosphorylation phenotype in TISCs, which is needed for the production of metabolites during tumor cell differentiation and proliferation. The infiltrating CD8 and CD4 T-lymphocytes in P4 tumors demonstrated increased expression of the immune checkpoint inhibitor (ICI) CTLA4, a known binding partner of CD80, to cause immune exhaustion and pro-tumorigenic effects. Interestingly, anti-TGFβ monoclonal antibodies (mAbs) played a synergistic role in further enhancing the anti-tumor effect of anti-CTLA4 mAb. In summary, our findings demonstrated that chronic HS diet increased the frequency of TISCs in tumors leading to blunting of cytotoxic adaptive immune responses causing tumor proliferation. Furthermore, a combination of anti-TGFβ with current ICI-based immunotherapies could exert more favorable anti-cancer clinical outcomes.
Product Citations: 25
Chronic High-Salt Diet Activates Tumor-Initiating Stem Cells Leading to Breast Cancer Proliferation.
In Cells on 25 May 2024 by Tucker, L., Ali, U., et al.
-
FC/FACS
-
Mus musculus (House mouse)
-
Cancer Research
-
Cell Biology
-
Stem Cells and Developmental Biology
Tuning DNA Dissociation from Spherical Nucleic Acids for Enhanced Immunostimulation.
In ACS Nano on 26 September 2023 by Dittmar, J. W., Teplensky, M. H., et al.
The stability of the core can significantly impact the therapeutic effectiveness of liposome-based drugs. While the spherical nucleic acid (SNA) architecture has elevated liposomal stability to increase therapeutic efficacy, the chemistry used to anchor the DNA to the liposome core is an underexplored design parameter with a potentially widespread biological impact. Herein, we explore the impact of SNA anchoring chemistry on immunotherapeutic function by systematically studying the importance of hydrophobic dodecane anchoring groups in attaching DNA strands to the liposome core. By deliberately modulating the size of the oligomer that defines the anchor, a library of structures has been established. These structures, combined with in vitro and in vivo immune stimulation analyses, elucidate the relationships between and importance of anchoring strength and dissociation of DNA from the SNA shell on its biological properties. Importantly, the most stable dodecane anchor, (C12)9, is superior to the n = 4-8 and 10 structures and quadruples immune stimulation compared to conventional cholesterol-anchored SNAs. When the OVA1 peptide antigen is encapsulated by the (C12)9 SNA and used as a therapeutic vaccine in an E.G7-OVA tumor model, 50% of the mice survived the initial tumor, and all of those survived tumor rechallenge. Importantly, the strong innate immune stimulation does not cause a cytokine storm compared to linear immunostimulatory DNA. Moreover, a (C12)9 SNA that encapsulates a peptide targeting SARS-CoV-2 generates a robust T cell response; T cells raised from SNA treatment kill >40% of target cells pulsed with the same peptide and ca. 45% of target cells expressing the entire spike protein. This work highlights the importance of using anchor chemistry to elevate SNA stability to achieve more potent and safer immunotherapeutics in the context of both cancer and infectious disease.
-
Mus musculus (House mouse)
-
Genetics
In Nature Communications on 16 November 2022 by Darragh, L. B., Gadwa, J., et al.
In the setting of conventional radiation therapy, even when combined with immunotherapy, head and neck cancer often recurs locally and regionally. Elective nodal irradiation (ENI) is commonly employed to decrease regional recurrence. Given our developing understanding that immune cells are radio-sensitive, and that T cell priming occurs in the draining lymph nodes (DLNs), we hypothesize that radiation therapy directed at the primary tumor only will increase the effectiveness of immunotherapies. We find that ENI increases local, distant, and metastatic tumor growth. Multi-compartmental analysis of the primary/distant tumor, the DLNs, and the blood shows that ENI decreases the immune response systemically. Additionally, we find that ENI decreases antigen-specific T cells and epitope spreading. Treating the primary tumor with radiation and immunotherapy, however, fails to reduce regional recurrence, but this is reversed by either concurrent sentinel lymph node resection or irradiation. Our data support using lymphatic sparing radiation therapy for head and neck cancer.
© 2022. The Author(s).
-
Mus musculus (House mouse)
-
Cancer Research
-
Immunology and Microbiology
DnaJ, a promising vaccine candidate against Ureaplasma urealyticum infection.
In Applied Microbiology and Biotechnology on 1 November 2022 by Guo, F., Tang, Y., et al.
Ureaplasma urealyticum (U. urealyticum, Uu) is a common sexually transmitted pathogen that is responsible for diseases such as non-gonococcal urethritis, chorioamnionitis, and neonatal respiratory diseases. The rapid emergence of multidrug-resistant bacteria threatens the effective treatment of Uu infections. Considering this, vaccination could be an efficacious medical intervention to prevent Uu infection and disease. As a highly conserved molecular chaperone, DnaJ is expressed and upregulated by pathogens soon after infection. Here, we assessed the vaccine potential of recombinant Uu-DnaJ in a mouse model and dendritic cells. Results showed that intramuscular administration of DnaJ induced robust humoral- and T helper (Th) 1 cell-mediated immune responses and protected against genital tract infection, inflammation, and the pathologic sequelae after Uu infection. Importantly, the DnaJ protein also induced the maturation of mouse bone marrow-derived dendritic cells (BMDCs), ultimately promoting naïve T cell differentiation toward the Th1 phenotype. In addition, adoptive immunization of DnaJ-pulsed BMDCs elicited antigen-specific Immunoglobulin G2 (IgG2) antibodies as well as a Th1-biased cellular response in mice. These results support DnaJ as a promising vaccine candidate to control Uu infections. KEY POINTS: • A novel recombinant vaccine was constructed against U. urealyticum infection. • Antigen-specific humoral and cellular immune responses after DnaJ vaccination. • Dendritic cells are activated by Uu-DnaJ, which results in a Th1-biased immune response.
© 2022. The Author(s), under exclusive licence to Springer-Verlag GmbH Germany, part of Springer Nature.
-
Mus musculus (House mouse)
-
Immunology and Microbiology
DnaJ, A Promising Vaccine Candidate Against Ureaplasma Urealyticum Infection
Preprint on Research Square on 6 December 2021 by Guo, F., Tang, Y., et al.
h4>Background: /h4> Ureaplasma urealyticum (Uu) is an important sexually transmitted pathogen that is responsible for diseases such as non-gonococcal urethritis, chorioamnionitis and neonatal respiratory diseases. The rapid emergence of multidrug-resistant bacteria threatens the effective treatment of U. urealyticum infections. Considering this, vaccination could be an efficacious medical intervention to prevent U. urealyticum infection and disease. As a highly conserved molecular chaperone, DnaJ is expressed and upregulated by pathogens soon after infection. Here, we assessed the potential of recombinant DnaJ vaccine in a mouse model and dendritic cells (DCs). h4>Results: /h4>: The results showed that intramuscular administration of recombinant DnaJ induced robust humoral- and T helper (Th) 1 cell-mediated immune responses and protected against cervical infection, inflammation, and the pathologic sequelae after U. urealyticum infection. Importantly, DnaJ also induced the maturation of mouse bone marrow-derived DCs (BMDCs), ultimately promoting naïve T-cell differentiation towards the Th1 phenotype. In addition, adoptive immunisation of DnaJ-pulsed BMDCs elicited antigen-specific immunoglobulin G2 antibodies as well as a Th1-biased cellular response in mice. h4>Conclusion: /h4> We concluded that DnaJ can be a promising vaccine candidate to control U. urealyticum infections.
-
FC/FACS
-
Mus musculus (House mouse)
-
Immunology and Microbiology
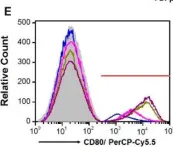
In Cells on 25 May 2024 by Tucker, L., Ali, U., et al.
Fig.5.E

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Cells by CiteAb, provided under a CC-BY license
Image 1 of 4
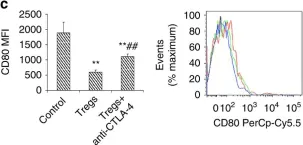
In Nat Commun on 29 September 2017 by Deliyanti, D., Talia, D. M., et al.
Fig.8.C

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 4
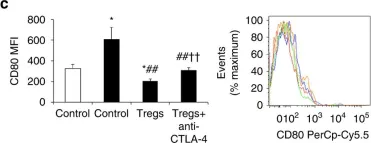
In Nat Commun on 29 September 2017 by Deliyanti, D., Talia, D. M., et al.
Fig.7.C

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 4
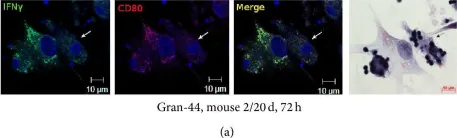
In J Immunol Res on 12 April 2016 by Ufimtseva, E.
Fig.6.A

-
ICC-IF
-
Mus musculus (House mouse)
Collected and cropped from J Immunol Res by CiteAb, provided under a CC-BY license
Image 1 of 4