The uterine smooth muscle (myometrium) is an immunomodulatory tissue capable of secreting multiple chemokines during pregnancy. We propose that before term labor, chemokines secreted as a result of mechanical stretch of the uterine walls by the growing fetus(es) induce infiltration of maternal monocytes into myometrium, drive their differentiation into macrophages, and induce pro-inflammatory (M1) polarization, leading to labor contractions. This study used high-throughput proteomic mass-spectrometry to investigate the underlying mechanisms and explored the therapeutic potential of a broad-spectrum chemokine inhibitor (BSCI, FX125L) in modulating these effects. Primary myocytes isolated from the myometrium of term pregnant women were subjected in vitro to static mechanical stretch. Proteomic analysis of stretched myocyte-conditioned media (CM) identified significant upregulation of chemokine-related pathways and ECM degradation proteins. CM induced in vitro differentiation of human monocytes to macrophages and polarization into an M1-like phenotype characterized by elevated ROS production. BSCI treatment altered the myocyte secretome, increasing tissue-remodeling and anti-inflammatory proteins, Annexin A1 and TGF-β. BSCI-treated myocyte secretions induced Annexin A1 expression in macrophages and enhanced their phagocytic activity. We conclude that factors secreted by mechanically stretched myocytes induce pro-inflammatory M1 macrophage polarization, while BSCI modulates myocyte secretome, which reprograms macrophages to a homeostatic M2-like phenotype, thus reducing inflammation. When treated with BSCI, M2-polarized macrophages reduced myocyte-driven collagen gel contraction, whereas M1 macrophages enhanced it. This study reveals novel insights into the myocyte-macrophage interaction and identifies BSCI as a promising drug to modulate myometrial activity. We suggest that uterine macrophages may represent a therapeutic target for preventing preterm labor in women.
Product Citations: 19
In Cells on 30 March 2025 by Boros-Rausch, A., Dorogin, A., et al.
-
Cell Biology
-
Immunology and Microbiology
Preprint on Research Square on 7 November 2024 by Zhang, X., Yang, J., et al.
Abstract Objective The long non-coding RNA (lncRNA) PVT1 plays a significant role in regulating the development and progression of various cancers. However, its clinical relevance in triple-negative breast cancer (TNBC) and its immunoregulatory mechanisms in TNBC remain largely unexplored. Methods An orthotopic TNBC mouse model was established, and single-cell RNA sequencing was performed on tumor tissues to examine macrophage populations. Bulk RNA sequencing, differential expression analysis, and Weighted Gene Co-expression Network Analysis were integrated to identify key factors of interest. Experiments using the co-culture si-PVT1-transduced oe-PPARγ TNBC cells with macrophages were conducted to observe their effects on TNBC cell growth and on M1/M2 marker expression both in vivo and in vitro. Additionally, the interactions of PVT1, NOP56, and E2F1 and their influence on PPARγ transcription were analyzed using RNA/DNA immunoprecipitation, ChIP-qPCR, and luciferase reporter assays. Results Macrophage reprogramming occurred in the TNBC tissues of mice, characterized by a significant accumulation of M2-type macrophages in tumor tissues. Both PVT1 and PPARγ play pivotal roles in this reprogramming. PVT1 knockdown (KD) suppressed the expression of PPARγ and M2 macrophage markers, while oe-PPARγ partially restored M2 marker expression. In vitro, PVT1 enhances TNBC cell proliferation, invasion, and metastasis through PPARγ. Similarly, in vivo, PVT1 promotes TNBC tumor growth and M2 marker expression via PPARγ. Mechanistically, PVT1 functions as a scaffold to recruit NOP56 and E2F1, forming a PVT1–NOP56–E2F1 complex that facilitates the transcriptional upregulation of PPARγ. Conclusion LncRNA PVT1 significantly affects macrophage polarization and TNBC progression by regulating PPARγ transcription. These findings suggest novel molecular targets for TNBC therapy development.
-
Biochemistry and Molecular biology
-
Cancer Research
-
Immunology and Microbiology
In Neural Regeneration Research on 1 November 2024 by Ding, Y., Sun, Y., et al.
JOURNAL/nrgr/04.03/01300535-202419110-00029/figure1/v/2024-03-08T184507Z/r/image-tiff Our previous study has demonstrated that lnc_000048 is upregulated in large-artery atherosclerotic stroke and promotes atherosclerosis in ApoE-/- mice. However, little is known about the role of lnc_000048 in classically activated macrophage (M1) polarization. In this study, we established THP-1-derived testing state macrophages (M0), M1 macrophages, and alternately activated macrophages (M2). Real-time fluorescence quantitative PCR was used to verify the expression of marker genes and the expression of lnc_000048 in macrophages. Flow cytometry was used to detect phenotypic proteins (CD11b, CD38, CD80). We generated cell lines with lentivirus-mediated upregulation or downregulation of lnc_000048. Flow cytometry, western blot, and real-time fluorescence quantitative PCR results showed that down-regulation of lnc_000048 reduced M1 macrophage polarization and the inflammation response, while over-expression of lnc_000048 led to the opposite effect. Western blot results indicated that lnc_000048 enhanced the activation of the STAT1 pathway and mediated the M1 macrophage polarization. Moreover, catRAPID prediction, RNA-pull down, and mass spectrometry were used to identify and screen the protein kinase RNA-activated (PKR), then catRAPID and RPIseq were used to predict the binding ability of lnc_000048 to PKR. Immunofluorescence (IF)-RNA fluorescence in situ hybridization (FISH) double labeling was performed to verify the subcellular colocalization of lnc_000048 and PKR in the cytoplasm of M1 macrophage. We speculate that lnc_000048 may form stem-loop structure-specific binding and activate PKR by inducing its phosphorylation, leading to activation of STAT1 phosphorylation and thereby enhancing STAT1 pathway-mediated polarization of THP-1 macrophages to M1 and inflammatory factor expression. Taken together, these results reveal that the lnc_000048/PKR/STAT1 axis plays a crucial role in the polarization of M1 macrophages and may be a novel therapeutic target for atherosclerosis alleviation in stroke.
Copyright © 2024 Copyright: © 2024 Neural Regeneration Research.
-
Homo sapiens (Human)
-
Neuroscience
In Scientific Reports on 10 September 2024 by Hansen, F. J., Mittelstädt, A., et al.
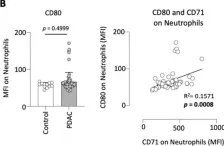
Pancreatic ductal adenocarcinoma (PDAC) is one of the most lethal malignancies, presenting a persisting global health burden. Neutrophils have a double-edged role in tumor progression exhibiting both pro-tumor and anti-tumor functions. CD71, also known as transferrin receptor 1, performs a critical role in cellular iron uptake and is highly expressed on proliferating cells, and especially on activated immune cells. CD71 is known to be elevated in various types of solid cancers and is associated with poor prognosis, however, the expression of CD71 on neutrophils in PDAC and its potential clinical impact is still unknown. Therefore, we analyzed CD71 on circulating neutrophils in PDAC and clinical control patients and found a significant increased expression in PDAC patients. High expression of CD71 on neutrophils in PDAC patients was associated with reduced outcome compared to low expression. CD71 on neutrophils correlated positively with the levels of proinflammatory cytokines IL-6, IFN-γ, and growth factor ligands CD40-L, and BAFF in plasma of PDAC patients. Finally, we have demonstrated that high expression of CD71 on neutrophils was also associated with an increased expression of CD39 and CD25 on circulating T-cells. Based on our findings, we hypothesize that CD71 on neutrophils is associated with tumor progression in PDAC. Further studies are required to investigate the distinct functionality of CD71 expressing neutrophils and their potential clinical application.
© 2024. The Author(s).
-
FC/FACS
-
Homo sapiens (Human)
-
Cancer Research
In IScience on 16 August 2024 by Parveen, S., Bhat, C. V., et al.
Streptococcus pneumoniae is a global priority respiratory pathogen that kills over a million people annually. The pore-forming cytotoxin, pneumolysin (PLY) is a major virulence factor. Here, we found that recombinant PLY as well as wild-type pneumococcal strains, but not the isogenic PLY mutant, upregulated the shedding of extracellular vesicles (EVs) harboring membrane-bound toxin from human THP-1 monocytes. PLY-EVs induced cytotoxicity and hemolysis dose-dependently upon internalization by recipient monocyte-derived dendritic cells. Proteomics analysis revealed that PLY-EVs are selectively enriched in key inflammatory host proteins such as IFI16, NLRC4, PTX3, and MMP9. EVs shed from PLY-challenged or infected cells induced dendritic cell maturation and primed them to infection. In vivo, zebrafish administered with PLY-EVs showed pericardial edema and mortality. Adoptive transfer of bronchoalveolar-lavage-derived EVs from infected mice to healthy recipients induced lung damage and inflammation in a PLY-dependent manner. Our findings identify that host EVs released during infection mediate pneumococcal pathogenesis.
© 2024 The Author(s).
-
Immunology and Microbiology
In Sci Rep on 10 September 2024 by Hansen, F. J., Mittelstädt, A., et al.
Fig.2.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Sci Rep by CiteAb, provided under a CC-BY license
Image 1 of 2
In Front Immunol on 20 April 2021 by Lin, S., Cheng, L., et al.
Fig.4.B

-
FC/FACS
-
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 2