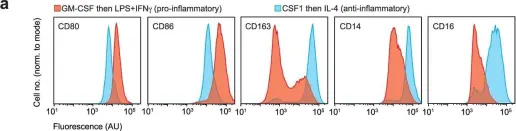
Inflammation is a complex physiological process triggered in response to harmful stimuli1. It involves cells of the immune system capable of clearing sources of injury and damaged tissues. Excessive inflammation can occur as a result of infection and is a hallmark of several diseases2-4. The molecular bases underlying inflammatory responses are not fully understood. Here we show that the cell surface glycoprotein CD44, which marks the acquisition of distinct cell phenotypes in the context of development, immunity and cancer progression, mediates the uptake of metals including copper. We identify a pool of chemically reactive copper(II) in mitochondria of inflammatory macrophages that catalyses NAD(H) redox cycling by activating hydrogen peroxide. Maintenance of NAD+ enables metabolic and epigenetic programming towards the inflammatory state. Targeting mitochondrial copper(II) with supformin (LCC-12), a rationally designed dimer of metformin, induces a reduction of the NAD(H) pool, leading to metabolic and epigenetic states that oppose macrophage activation. LCC-12 interferes with cell plasticity in other settings and reduces inflammation in mouse models of bacterial and viral infections. Our work highlights the central role of copper as a regulator of cell plasticity and unveils a therapeutic strategy based on metabolic reprogramming and the control of epigenetic cell states.
© 2023. The Author(s).
Product Citations: 6
A druggable copper-signalling pathway that drives inflammation.
In Nature on 1 May 2023 by Solier, S., Müller, S., et al.
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
In The EMBO Journal on 1 March 2023 by Kennedy, A., Robinson, M. A., et al.
CTLA-4 and PD-1 are key immune checkpoint receptors that are targeted in the treatment of cancer. A recently identified physical interaction between the respective ligands, CD80 and PD-L1, has been shown to block PD-L1/PD-1 binding and to prevent PD-L1 inhibitory functions. Since CTLA-4 is known to capture and degrade its ligands via transendocytosis, we investigated the interplay between CD80 transendocytosis and CD80/PD-L1 interaction. We find that transendocytosis of CD80 results in a time-dependent recovery of PD-L1 availability that correlates with CD80 removal. Moreover, CD80 transendocytosis is highly specific in that only CD80 is internalised, while its heterodimeric PD-L1 partner remains on the plasma membrane of the antigen-presenting cell (APC). CTLA-4 interactions with CD80 do not appear to be inhibited by PD-L1, but efficient removal of CD80 requires an intact CTLA-4 cytoplasmic domain, distinguishing this process from more general trogocytosis and simple CTLA-4 binding to CD80/PD-L1 complexes. These data are consistent with CTLA-4 acting as modulator of PD-L1:PD-1 interactions via control of CD80.
© 2023 The Authors. Published under the terms of the CC BY 4.0 license.
-
Immunology and Microbiology
Caspase Inhibition Modulates Monocyte-Derived Macrophage Polarization in Damaged Tissues.
In International Journal of Molecular Sciences on 19 February 2023 by Solier, S., Mondini, M., et al.
Circulating monocytes are recruited in damaged tissues to generate macrophages that modulate disease progression. Colony-stimulating factor-1 (CSF-1) promotes the generation of monocyte-derived macrophages, which involves caspase activation. Here, we demonstrate that activated caspase-3 and caspase-7 are located to the vicinity of the mitochondria in CSF1-treated human monocytes. Active caspase-7 cleaves p47PHOX at aspartate 34, which promotes the formation of the NADPH (nicotinamide adenine dinucleotide phosphate) oxidase complex NOX2 and the production of cytosolic superoxide anions. Monocyte response to CSF-1 is altered in patients with a chronic granulomatous disease, which are constitutively defective in NOX2. Both caspase-7 down-regulation and radical oxygen species scavenging decrease the migration of CSF-1-induced macrophages. Inhibition or deletion of caspases prevents the development of lung fibrosis in mice exposed to bleomycin. Altogether, a non-conventional pathway that involves caspases and activates NOX2 is involved in CSF1-driven monocyte differentiation and could be therapeutically targeted to modulate macrophage polarization in damaged tissues.
-
FC/FACS
-
Immunology and Microbiology
In Communications Biology on 19 May 2022 by Khan, A., Zhang, K., et al.
Mycobacterium tuberculosis (Mtb) is responsible for approximately 1.5 million deaths each year. Though 10% of patients develop tuberculosis (TB) after infection, 90% of these infections are latent. Further, mice are nearly uniformly susceptible to Mtb but their M1-polarized macrophages (M1-MΦs) can inhibit Mtb in vitro, suggesting that M1-MΦs may be able to regulate anti-TB immunity. We sought to determine whether human MΦ heterogeneity contributes to TB immunity. Here we show that IFN-γ-programmed M1-MΦs degrade Mtb through increased expression of innate immunity regulatory genes (Inregs). In contrast, IL-4-programmed M2-polarized MΦs (M2-MΦs) are permissive for Mtb proliferation and exhibit reduced Inregs expression. M1-MΦs and M2-MΦs express pro- and anti-inflammatory cytokine-chemokines, respectively, and M1-MΦs show nitric oxide and autophagy-dependent degradation of Mtb, leading to increased antigen presentation to T cells through an ATG-RAB7-cathepsin pathway. Despite Mtb infection, M1-MΦs show increased histone acetylation at the ATG5 promoter and pro-autophagy phenotypes, while increased histone deacetylases lead to decreased autophagy in M2-MΦs. Finally, Mtb-infected neonatal macaques express human Inregs in their lymph nodes and macrophages, suggesting that M1 and M2 phenotypes can mediate immunity to TB in both humans and macaques. We conclude that human MФ subsets show unique patterns of gene expression that enable differential control of TB after infection. These genes could serve as targets for diagnosis and immunotherapy of TB.
© 2022. The Author(s).
-
FC/FACS
-
Homo sapiens (Human)
-
Immunology and Microbiology
In Cell Reports on 17 March 2020 by Lim, C. X., Lee, B., et al.
DC-SIGN+ monocyte-derived dendritic cells (mo-DCs) play important roles in bacterial infections and inflammatory diseases, but the factors regulating their differentiation and proinflammatory status remain poorly defined. Here, we identify a microRNA, miR-181a, and a molecular mechanism that simultaneously regulate the acquisition of DC-SIGN expression and the activation state of DC-SIGN+ mo-DCs. Specifically, we show that miR-181a promotes DC-SIGN expression during terminal mo-DC differentiation and limits its sensitivity and responsiveness to TLR triggering and CD40 ligation. Mechanistically, miR-181a sustains ERK-MAPK signaling in mo-DCs, thereby enabling the maintenance of high levels of DC-SIGN and a high activation threshold. Low miR-181a levels during mo-DC differentiation, induced by inflammatory signals, do not support the high phospho-ERK signal transduction required for DC-SIGNhi mo-DCs and lead to development of proinflammatory DC-SIGNlo/- mo-DCs. Collectively, our study demonstrates that high DC-SIGN expression levels and a high activation threshold in mo-DCs are linked and simultaneously maintained by miR-181a.
Copyright © 2020. Published by Elsevier Inc.
-
Immunology and Microbiology
In Nature on 1 May 2023 by Solier, S., Müller, S., et al.
Fig.1.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nature by CiteAb, provided under a CC-BY license
Image 1 of 2
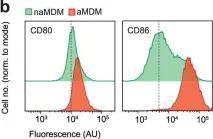
In Nature on 1 May 2023 by Solier, S., Müller, S., et al.
Fig.1.B

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nature by CiteAb, provided under a CC-BY license
Image 1 of 2