The close association between nasopharyngeal carcinoma (NPC) and Epstein-Barr virus (EBV) infection highlights the potential of therapeutic vaccination against viral antigens as an attractive immunotherapy for treating EBV+ NPC. Maximizing vaccine efficacy often requires selecting optimal T cell epitopes and incorporating co-treatment strategies. Here, we analyzed genomic mutations of 283 cancer-associated EBV strains and predicted epitopes with broad human leukocyte antigen (HLA) coverage from high-frequency nonsynonymous mutations. A polyepitope mRNA vaccine constructed from the predicted epitopes elicited antigen-specific T cell responses but showed suboptimal efficacy in tumor control in a PBMC-humanized mouse EBV+ NPC model. To enhance treatment efficacy, we developed an optimized system for expanding human natural killer (NK) cells with high purity and cytotoxicity as a co-treatment modality. Combined administration of mRNA vaccine and NK cells synergistically improved therapeutic efficacy by durably suppressing or eradicating NPC tumors in humanized mice. The concurrent treatment could improve the infiltration of both human T cells and NK cells into the tumor microenvironment and boost their effector functions. Our study suggests the combined therapeutic vaccination and NK cell therapy as a potential strategy for treating EBV+ NPC.
© 2025 The Author(s).
Product Citations: 72
In Molecular Therapy. Oncology on 18 June 2025 by Huang, K., Lin, X. J., et al.
-
Cancer Research
-
Genetics
-
Immunology and Microbiology
In Cancer Pathogenesis and Therapy on 1 May 2025 by Hu, X., Ouyang, W., et al.
Gastric cancer (GC) is a common malignancy characterized by the absence of reliable prognostic indicators and effective therapeutic targets. Claudin-9 (CLDN9) has been demonstrated to be upregulated in various cancers. However, its prognostic value, biological function, and regulatory mechanisms in GC remain unclear. Therefore, this study aimed to elucidate the role of CLDN9 in GC progression and its underlying mechanisms.
We utilized consensus cluster, random survival forest, and multivariate Cox regression analyses to identify CLDN9 in GC. Subsequently, we evaluated the mRNA and protein levels of CLDN9 in GC using quantitative real-time polymerase chain reaction (PCR) (qRT-PCR), Western blotting (WB), and immunohistochemistry (IHC). Furthermore, the role of CLDN9 in GC progression was investigated using a series of functional in vivo and in vitro experiments. Finally, we elucidated the molecular mechanisms of CLDN9 using bioinformatics, molecular biology, animal models, and patient tissue specimens.
Two GC subtypes with survival and functional differences were identified based on glycolytic metabolic genes in the Cancer Genome Atlas (TCGA)- Stomach adenocarcinoma (STAD) dataset. A prognostic risk score was calculated using seven genes to assess the overall survival (OS) in GC. Using random survival forest and multivariate Cox analyses, we identified CLDN9 as the key gene linked to the glycolytic subtype and prognosis of GC. CLDN9 expression was significantly upregulated in patients with GC as well as in GC cells. CLDN9 knockdown inhibited tumor proliferation, invasion, and metastasis both in vivo and in vitro. Mechanistically, CLDN9 was found to regulate lactate dehydrogenase A (LDHA) expression and promote glycolytic metabolism by activating the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT)/hypoxia-inducible factor 1-alpha (HIF1α) signaling pathway. Additionally, lactate, a glycolytic metabolite, enhanced programmed cell death ligand 1 (PD-L1) lactylation and stability, which suppressed anti-tumor immunity in CD8+ T cells, thereby contributing to GC progression.
CLDN9 expression is associated with GC development and progression. Mechanistically, CLDN9 enhances the glycolysis pathway and facilitates PD-L1 lactylation through the PI3K/AKT/HIF1α signaling pathway, thereby suppressing anti-tumor immunity in CD8+ T cells. CLDN9 has the potential to serve as a novel prognostic marker and therapeutic target for GC.
© 2024 Published by Elsevier B.V. on behalf of Chinese Medical Association (CMA).
-
Cancer Research
-
Immunology and Microbiology
In IScience on 18 April 2025 by Liu, H., Ge, W., et al.
Hepatocellular carcinoma (HCC) resists immunotherapy due to its immunosuppressive microenvironment. Sarcoma homology 2 domain-containing protein tyrosine phosphatase-1 (SHP-1) inhibits T cell receptor signaling, and its pharmacological inhibition is limited by poor selectivity and membrane permeability. Here, we generated CRISPR-edited SHP-1-knockout (KO) CD8+ T cells to enhance adoptive therapy against HCC. Single-cell RNA sequencing of HCC patient T cells revealed elevated SHP-1 in exhausted subsets. SHP-1-KO T cells exhibited increased effector memory T cells (TEM) proportions and enhanced IFN-γ/Granzyme B/perforin secretion, improving cytotoxicity against HCC lines. In humanized PDX models, SHP-1-KO T cells demonstrated superior tumor-killing activity. Transcriptomics identified upregulated lipid metabolism pathways, with HMGCR as a hub gene. Combining SHP-1-KO T cells with simvastatin (HMGCR inhibitor) synergistically amplified anti-HCC efficacy. This study proposes a dual strategy combining SHP-1-targeted cell therapy and metabolic modulation to overcome immunotherapy resistance, offering a translatable approach for HCC treatment.
© 2025 The Author(s).
-
Cancer Research
In Acta Pharmaceutica Sinica. B on 1 April 2025 by Li, S., Liu, Y., et al.
The Janus kinase/signal transducers and activators of transcription (JAK-STAT) control natural killer (NK) cells development and cytotoxic functions, however, whether long non-coding RNAs (lncRNAs) are involved in this pathway remains unknown. We found that miR155HG was elevated in activated NK cells and promoted their proliferation and effector functions in both NK92 and induced-pluripotent stem cells (iPSCs)-derived NK (iPSC-NK) cells, without reliance on its derived miR-155 and micropeptide P155. Mechanistically, miR155HG bound to miR-6756 and relieved its repression of JAK3 expression, thereby promoting the JAK-STAT pathway and enhancing NK cell proliferation and function. Further investigations disclosed that upon cytokine stimulation, STAT3 directly interacts with miR155HG promoter and induces miR155HG transcription. Collectively, we identify a miR155HG-mediated positive feedback loop of the JAK-STAT signaling. Our study will also provide a power target regarding miR155HG for improving NK cell generation and effector function in the field of NK cell adoptive transfer therapy against cancer, especially iPSC-derived NK cells.
© 2025 The Authors.
MAIT Cells in the Bone Marrow of Patients with Aplastic Anemia.
In International Journal of Molecular Sciences on 21 September 2024 by Lam, V. Q., Espinoza, J. L., et al.
Mucosal-associated invariant T cells (MAIT cells) are a subset of T cells with innate, effector-like properties that play an essential role in the immune response to microbial infections. In humans, MAIT cells are detectable in the blood, liver, and lungs, but little is known about the frequency of these cells in the bone marrow. Also, the pathogenic role, if any, of MAIT cells in the development of aplastic anemia, a disease with an exquisite origin in the bone marrow, is currently unknown. We investigated the frequency and clinical relevance of bone marrow MAIT cells in a cohort of 14 patients (60.6 ± 23 and 57% women) with aplastic anemia. MAIT cells in the bone marrow samples obtained at diagnosis were evaluated by flow cytometry, and their association with various blood cell parameters and the patients' clinical features was analyzed. MAIT cells were detectable in the bone marrow of all patients, with considerable variations among them. Bone marrow MAIT cells expressing the activator receptor natural killer group 2D - NKG2D (NKG2D+ MAIT cells) were significantly more abundant in the specimens of the aplastic anemia patients than in patients with bone marrow failure distinct from aplastic anemia. In addition, the NKG2D+ MAIT cells positively correlated with whole blood cell counts (WBC), platelet counts, and neutrophil counts, as well as with various inflammatory markers, including neutrophil-to-lymphocyte rate (NLR), platelet-to-lymphocyte rate (PLR), and systemic inflammatory index (SII). In functional studies, bone marrow CD34+ hematopoietic cells exposed to phytohemagglutinin or bacterial-derived lipopolysaccharide and acetyl-6-formylpterin upregulated MR1 (major histocompatibility complex, class I-related, known to interact with MAIT cells) and MICA/B (MHC class I chain-related gene A, a ligand of NKG2D) proteins on their cell surface, suggesting that under stress conditions, CD34+ hematopoietic cells are more likely to interact with NKG2D+ MAIT cells. In addition, NKG2D+ MAIT cells upregulated perforin and granzyme B in response to their interaction with recombinant MICA protein in vitro. This study reports for the first time the frequency of MAIT cells in the bone marrow of patients with aplastic anemia and assesses the potential implications of these cells in the pathogenesis or progression of aplastic anemia.
-
Homo sapiens (Human)
In J Immunother Cancer on 1 April 2021 by Wang, G., Zhou, X., et al.
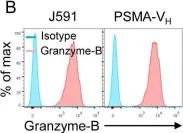
Fig.2.B

-
FC/FACS
-
Collected and cropped from J Immunother Cancer by CiteAb, provided under a CC-BY license
Image 1 of 1