Exosomes can be used to mediate the delivery of nucleic acids such as microRNA-125b-5p (miR-125b-5p), a tumor-suppressor in certain types of cancer, into tumor cells. The present study investigated the use of bone mesenchymal stem cells-derived exosome (BMSCs-Exo) delivery of miR-125b-5p in ovarian cancer (OC). BMSCs were transfected with miR-125b-5p mimic, from which exosomes termed Exo-miR-125b-5p mimic were extracted. The expression levels of miR-125b-5p in OC tissue samples, BMSCs, exosomes and SKOV3 cells were quantified using reverse transcription-quantitative PCR. The influence of Exo-miR-125b-5p mimic on the biological functions of OC was evaluated through cell proliferation, invasion, migration and apoptosis assays. The targeting relationship between miR-125b-5p and DEAD-box helicase 5 (DDX5) was verified, and the expression levels of DDX5 in OC samples and SKOV3 cells were quantified using western blotting. miR-125b-5p was downregulated in tumor tissue samples from patients with OC. BMSCs-Exo reduced the malignant properties of SKOV3 cells in vitro, and these effects were be advanced by miR-125b-5p upregulation. miR-125b-5p targeted and inhibited DDX5 expression. DDX5 overexpression inhibited Exo-miR-125b-5p-induced suppression of OC development. Overall, this study highlights that BMSCs-Exo-encapsulated miR-125b-5p inhibited OC progression via DDX5 downregulation, providing insight into the molecular mechanisms underlying OC.
Copyright: © 2025 Wang et al.
Product Citations: 31
In Oncology Letters on 1 May 2025 by Wang, Y., Wang, W., et al.
-
Cancer Research
-
Stem Cells and Developmental Biology
In BMC Oral Health on 18 September 2024 by El Qashty, R. M. N., Youssef, J. M., et al.
Tongue defects have several etiologies and significantly affect the quality of life. This study was conducted to compare the regenerative potential of erythropoietin (EPO)-loaded hydrogel and adipose derived stem cell (ADSC) secretome on tongue dorsum defects focusing on the role of anti-inflammatory M2 macrophage phenotype.
Rats were subjected to induction of mechanical circular defects on the dorsal surface of the tongue, then divided into three groups; Group I (control): received 0.1 ml phosphate buffered saline, Group II (EPO): received 5000 U/kg EPO-hydrogel, and Group III (ADSC-Secretome): received 0.1 ml ADSC-Secretome. Treatments were injected circumferentially around wound margins after induction. Seven and fourteen days after treatment, specimens were obtained and processed for histological and immunohistochemical staining followed by the relevant histomorphometric and statistical analyses.
Seven days after treatment, groups II and III presented defects with some epithelial regeneration at the lateral margins, while the center of the defect showed granulation tissue with much inflammatory cells. The base of the defects showed some muscle fibers and new blood vessels, however group III showed more enhanced neovascularization. Fourteen days after therapeutic intervention, group II defects were completely covered with epithelium showing a thin keratin layer with regular rete pegs interdigitating with the underlying connective tissue papillae, but tongue papillae were not restored. Group III expressed much better healing with developing filiform papillae. The connective tissue showed more vascularity and well-arranged muscle bundles. Both treated groups showed a significant decrease in defect depth and significant increase in anti-inflammatory macrophages compared to the control group at both time intervals, however there was no significant difference between the two treated groups.
Both treatments showed promising and comparable results in the treatment of tongue defects reducing inflammation and restoring tongue histological architecture with significant upregulation of M2 macrophage.
© 2024. The Author(s).
-
Rattus norvegicus (Rat)
-
Endocrinology and Physiology
-
Stem Cells and Developmental Biology
In Organogenesis on 31 December 2023 by Hisanaga, M., Tsuchiya, T., et al.
Decellularized scaffolds are promising biomaterials for tissue and organ reconstruction; however, strategies to effectively suppress the host immune responses toward these implants, particularly those without chemical crosslinking, remain warranted. Administration of mesenchymal stem cells is effective against immune-mediated inflammatory disorders. Herein, we investigated the effect of isogeneic abdominal adipose-derived mesenchymal stem/stromal cells (ADMSCs) on xenogeneic biomaterial-induced immunoreactions. Peripheral bronchi from pigs, decellularized using a detergent enzymatic method, were engrafted onto tracheal defects of Brown Norway (BN) rats. BN rats were implanted with native pig bronchi (Xenograft group), decellularized pig bronchi (Decellularized Xenograft), or Decellularized Xenograft and ADMSCs (Decellularized Xenograft+ADMSC group). In the latter group, ADMSCs were injected intravenously immediately post implantation. Harvested graft implants were assessed histologically and immunohistochemically. We found that acute rejections were milder in the Decellularized Xenograft and Decellularized Xenograft+ADMSC groups than in the Xenograft group. Mild inflammatory cell infiltration and reduced collagen deposition were observed in the Decellularized Xenograft+ADMSC group. Additionally, ADMSC administration decreased CD8+ lymphocyte counts but increased CD163+ cell counts. In the Decellularized Xenograft+ADMSC group, serum levels of vascular endothelial growth factor and IL-10 were elevated and tissue deposition of IgM and IgG was low. The significant immunosuppressive effects of ADMSCs illustrate their potential use as immunosuppressive agents for xenogeneic biomaterial-based implants.
-
Rattus norvegicus (Rat)
-
Immunology and Microbiology
-
Stem Cells and Developmental Biology
-
Veterinary Research
In Cell Transplantation on 11 November 2023 by Tanoue, Y., Tsuchiya, T., et al.
Cell therapy using mesenchymal stromal cells (MSCs) is being studied for its immunosuppressive effects. In organ transplantation, the amount of MSCs that accumulate in transplanted organs and other organs may differ depending on administration timing, which may impact their immunosuppressive effects. In vitro, adipose-derived mesenchymal stem cells (ADMSCs) suppress lymphocyte activation under cell-to-cell contact conditions. However, in vivo, it is controversial whether ADMSCs are more effective in accumulating in transplanted organs or in secondary lymphoid organs. Herein, we aimed to investigate whether the timing of ADMSC administration affects its immunosuppression ability in a rat lung transplantation model. In the transplantation study, rats were intramuscularly administered half the usual dose of tacrolimus (0.5 mg/kg) every 24 h after lung transplantation. ADMSCs (1 × 106) were administered via the jugular vein before (PreTx) or after (PostTx) transplantation. Cell tracking using quantum dots was performed. ADMSCs accumulated predominantly in the lung and liver; fewer ADMSCs were distributed in the grafted lung in the PreTx group than in the PostTx group. The rejection rate was remarkably low in the ADMSC-administered groups, particularly in the PostTx group. Serum tumor necrosis factor-α (TNF-α), interferon-γ, and interleukin (IL)-6 levels showed a greater tendency to decrease in the PreTx group than in the PostTx group. The proportion of regulatory T cells in the grafted lung 10 days after transplantation was higher in the PostTx group than in the PreTx group. PostTx administration suppresses rejection better than PreTx administration, possibly due to regulatory T cell induction by ADMSCs accumulated in the transplanted lungs, suggesting a mechanism different from that in heart or kidney transplantation that PreTx administration is more effective than PostTx administration. These results could help establish cell therapy using MSCs in lung transplantation.
In BMC Oral Health on 5 October 2023 by El Qashty, R. M. N., Elkashty, O. A., et al.
Temporomandibular joint (TMJ) arthritis is a debilitating, challenging condition and different methods have been implicated for its treatment. This study aimed to test the therapeutic potentials of low-level laser therapy (LLLT) associated with adipose derived stem cells (ADSC) or their derived secretome on a murine model induced arthritis.
Forty eight rats were divided into four groups where group I was the sham control, the rest of animals were subjected to arthritis induction using complete Freund's adjuvant, then divided as follows: group II received phosphate buffered saline (PBS) intraarticular injection and irradiation of 0 j/cm2, group III received ADSCs derived secretome and irradiation of 38 j/cm2, and group IV received ADSCs and irradiation of 38 j/cm2 as well. One and three weeks after treatment, animals were euthanized, and paraffin blocks were processed for histological assessment by hematoxylin and eosin stain with histomorphometrical analysis. Histochemical evaluation of joint proteoglycan content was performed through toluidine blue stain, and immunohistochemical staining by the proinflammatory marker tumor necrosis factor-α (TNF-α) was performed followed by the relevant statistical tests.
The arthritis group showed histological signs of joint injury including cartilage atrophy, articular disc fibrosis, irregular osteochondral interface, and condylar bone resorption together with high inflammatory reaction and defective proteoglycan content. In contrast, the treated groups III and IV showed much restoration of the joint structure with normal cartilage and disc thickness. The inflammation process was significantly suppressed especially after three weeks as confirmed by the significant reduction in TNF-α positive immunostaining compared to the arthritic group, and the cartilage proteoglycan content also showed significant increase relative to the arthritic group. However, no significant difference between the results of the two treated groups was detected.
LLLT conjugated with ADSCs or ADSCs derived secretome can efficiently enhance the healing of arthritic TMJs. Stem cell secretome can be applied as a safe, potent therapy. However, further investigations are required to unravel its mechanism of action and pave its way as a safe, novel, cell free therapy.
© 2023. BioMed Central Ltd., part of Springer Nature.
-
FC/FACS
-
Rattus norvegicus (Rat)
-
Stem Cells and Developmental Biology
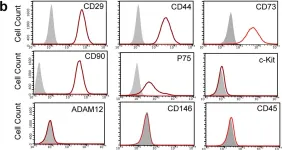
In Sci Rep on 10 January 2017 by Wang, D., Wang, A., et al.
Fig.3.B

-
FC/FACS
-
Rattus norvegicus (Rat)
Collected and cropped from Sci Rep by CiteAb, provided under a CC-BY license
Image 1 of 1