Microplastic particles from the air are inhaled and accumulate in the lungs, potentially causing immunological reactions and airway tissue injury. This study aimed to evaluate the biological effects of polyamide fibres on nasal epithelium co-cultivated with macrophages in control, asthma, and COPD groups. Nasal epithelial cells alone or in co-culture with monocyte-derived macrophages were exposed to polyamide fibres for 48 h. We identified 8 differentially expressed genes (DEGs) in controls, 309 DEGs in asthma (including ANKRD36C, BCL2L15, FCGBP, and IL-19), and 22 DEGs in COPD (e.g., BCL2L15, IL-19, CAPN14, PGBD5, PTPRH), particularly in epithelial/moMφ co-cultures. Microplastic exposure induced inflammatory cytokine secretion only for IL-8 production in controls (epithelial/ moMφs co-culture) and asthmatic (monoculture) epithelial cells in contrast to PM2.5, which was a strong inflammatory inducer. Gene Ontology analysis revealed that microplastic exposure affected sterol and cholesterol biosynthesis, secondary alcohol metabolism, and acetyl-CoA metabolism in asthma, and cell motility, chemokine signaling, leukocyte migration, and chemotaxis in COPD. Microplastic stimulation altered the response of airway epithelial cells in obstructive lung diseases differently than in controls, linking to Th2 inflammation, stress response modulation, and carcinogenesis. Asthmatic and COPD epithelial cells are more susceptible to damage from microplastic fibre exposure.
© 2025. The Author(s).
Product Citations: 11
The impaired response of nasal epithelial cells to microplastic stimulation in asthma and COPD.
In Scientific Reports on 4 February 2025 by Paplińska-Goryca, M., Misiukiewicz-Stępień, P., et al.
-
FC/FACS
-
Homo sapiens (Human)
In Respiratory Research on 8 January 2025 by Misiukiewicz-Stepien, P., Zajusz-Zubek, E., et al.
Pathobiology of asthma and chronic obstructive pulmonary disease (COPD) is associated with changes among respiratory epithelium structure and function. Increased levels of PM2.5 from urban particulate matter (UPM) are correlated with enlarged rate of asthma and COPD morbidity as well as acute disease exacerbation. It has been suggested that pre-existing pulmonary obstructive diseases predispose epithelium for different biological response than in healthy airways. The aim of this study was to assess the impact of PM2.5 on the biological response of healthy as well as asthma and COPD respiratory epithelium using 3D/spheroid culture model.
The spheroids from 5 healthy controls, 8 asthma patients, and 8 COPD patients were exposed to 100 µg/ml of PM2.5 for 24 h.
The common pattern for healthy asthma and COPD epithelium inflammatory response to PM2.5 stimulation include the increase in IL-1β, IL-6, IL-8 mRNA expression, and secretion of IL-6. Asthmatic spheroids produced higher amount of TNF-α and IL-8, whereas COPD spheroids expressed increased mRNA level of MUC5AC and decreased level of MMP7. PM2.5 treatment induced changes in AHR and TLR4 expression on secretory epithelium in COPD.
The response of airway epithelium to air pollution is different in healthy people than in obstructive lung disease patients. The impairment of airway epithelium in asthma and COPD changes their response to toxic environmental stimuli. This physiological dysfunction might be associated with diseases exacerbation of obstructive lung diseases.
© 2025. The Author(s).
-
FC/FACS
-
Homo sapiens (Human)
In Journal of Immunology Research on 8 May 2024 by Cevallos, C., Jarmoluk, P., et al.
This study aims to explore the influence of coinfection with HCV and HIV on hepatic fibrosis. A coculture system was set up to actively replicate both viruses, incorporating CD4 T lymphocytes (Jurkat), hepatic stellate cells (LX-2), and hepatocytes (Huh7.5). LX-2 cells' susceptibility to HIV infection was assessed through measurements of HIV receptor expression, exposure to cell-free virus, and cell-to-cell contact with HIV-infected Jurkat cells. The study evaluated profibrotic parameters, including programed cell death, ROS imbalance, cytokines (IL-6, TGF-β, and TNF-α), and extracellular matrix components (collagen, α-SMA, and MMP-9). The impact of HCV infection on LX-2/HIV-Jurkat was examined using soluble factors released from HCV-infected hepatocytes. Despite LX-2 cells being nonsusceptible to direct HIV infection, bystander effects were observed, leading to increased oxidative stress and dysregulated profibrotic cytokine release. Coculture with HIV-infected Jurkat cells intensified hepatic fibrosis, redox imbalance, expression of profibrotic cytokines, and extracellular matrix production. Conversely, HCV-infected Huh7.5 cells exhibited elevated profibrotic gene transcriptions but without measurable effects on the LX-2/HIV-Jurkat coculture. This study highlights how HIV-infected lymphocytes worsen hepatic fibrosis during HCV/HIV coinfection. They increase oxidative stress, profibrotic cytokine levels, and extracellular matrix production in hepatic stellate cells through direct contact and soluble factors. These insights offer valuable potential therapies for coinfected individuals.Copyright © 2024 Cintia Cevallos et al.
-
FC/FACS
-
Immunology and Microbiology
In BMC Complementary Medicine and Therapies on 2 June 2023 by Monika, P., Chandraprabha, M. N., et al.
Although chronic wounds are devastating and can cause burden at multiple levels, chronic wound research is still far behind. Chronic wound treatment is often less efficient due to delay in diagnosis and treatment, non-specific treatment mainly due to lack of knowledge of wound healing or healing resistance genes. It's known that chronic wounds do not progress towards healing, because it gets stalled in inflammatory phase of wound healing.
We aimed to use phytoextracts possessing excellent anti-inflammatory properties to regulate the unbalanced levels of cytokines responsible for increased inflammation.
Evaluation of anti-inflammatory activity of selected phytoextracts namely, Camellia sinensis (L.) Kuntze, Acacia catechu (L.f) Willd., Curcuma longa (L.), Allium sativum (L.), Punica granatum (L.) and Azadirachta indica A. hereafter, called as catechin, epicatechin, curcumin, garlic, pomegranate and neem extracts, respectively in Acute wound fibroblasts (AWFs) and Chronic wound fibroblasts (CWFs) using flow cytometry.
The phytoextracts exhibited no cytotoxicity below 100 μg/ml on normal Human Dermal fibroblasts (HDFs), while garlic extract showed highest cell viability followed by catechin, epicatechin, curcumin, pomegranate peel and neem based on IC50 value. Garlic, catechin and epicatechin extracts showed highest anti-inflammatory activities for both TGF-β and TNF-α in both AWFs and CWFs treated cells. After treatment of AWFs with catechin, epicatechin and garlic extracts, TGF-β and TNF-α expression was significantly reduced compared to untreated AWFs and reached to almost normal HDFs level. Also, after treatment of CWFs with catechin, epicatechin and garlic extracts, TGF-β and TNF-α expression was significantly reduced compared to untreated CWFs and was lesser than untreated AWFs.
The present findings reveal the potential of catechin, epicatechin and garlic extracts for the treatment of acute and chronic wounds with excellent anti-inflammatory properties.
© 2023. The Author(s).
-
Immunology and Microbiology
Pro- vs. Anti-Inflammatory Features of Monocyte Subsets in Glioma Patients.
In International Journal of Molecular Sciences on 18 January 2023 by Lehman, N., Kowalska, W., et al.
Monocytes constitute a heterogenous group of antigen-presenting cells that can be subdivided based on CD14, CD16 and SLAN expression. This division reflects the functional diversity of cells that may play different roles in a variety of pathologies including gliomas. In the current study, the three monocyte subpopulations: classical (CD14+ CD16+ SLAN-), intermediate (CD14dim CD16+ SLAN-) and non-classical (CD14low/- CD16+ SLAN+) in glioma patients' peripheral blood were analysed with flow cytometry. The immune checkpoint molecule (PD-1, PD-L1, SIRPalpha, TIM-3) expression along with pro- and anti-inflammatory cytokines (TNF, IL-12, TGF-beta, IL-10) were assessed. The significant overproduction of anti-inflammatory cytokines by intermediate monocytes was observed. Additionally, SLAN-positive cells overexpressed IL-12 and TNF when compared to the other two groups of monocytes. In conclusion, these results show the presence of different profiles of glioma patient monocytes depending on CD14, CD16 and SLAN expression. The bifold function of monocyte subpopulations might be an additional obstacle to the effectiveness of possible immunotherapies.
-
FC/FACS
-
Cancer Research
-
Immunology and Microbiology
In PLoS One on 26 May 2017 by Mishra, A. K., Parish, C. R., et al.
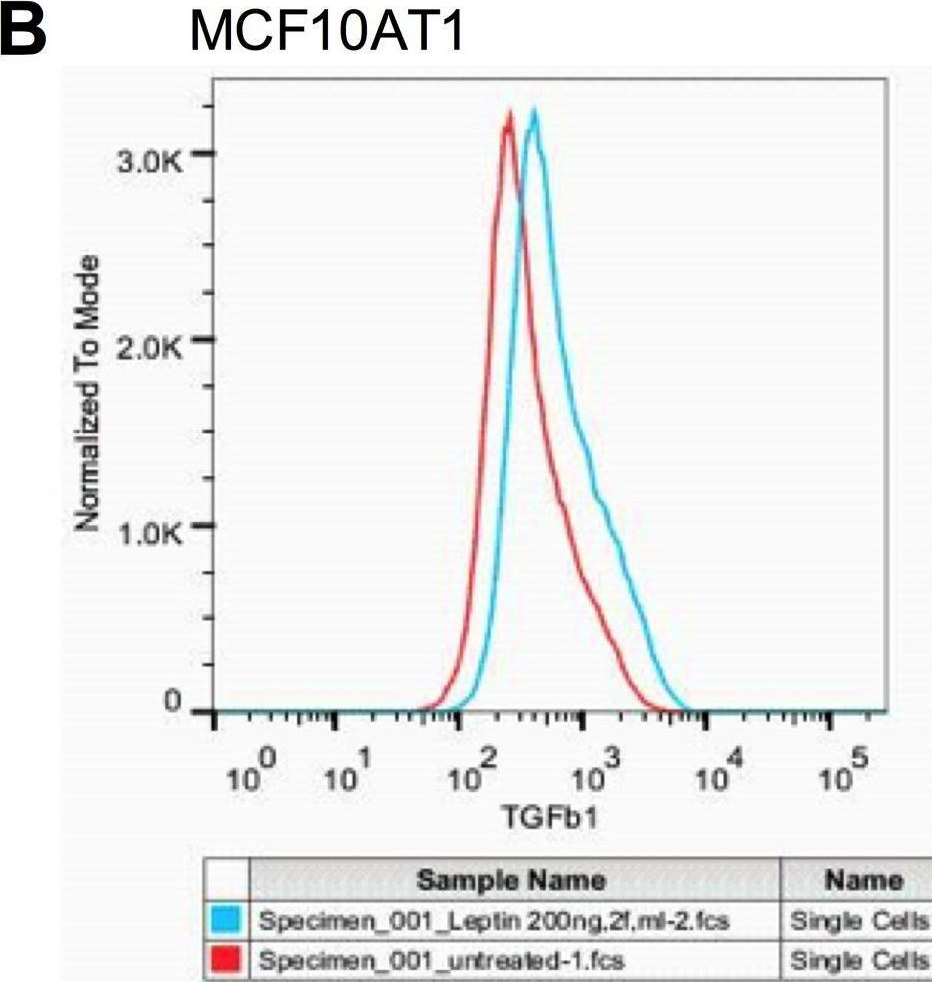
Fig.6.B
-
FC/FACS
-
Collected and cropped from PLoS ONE by CiteAb, provided under a CC-BY license
Image 1 of 1
