The concept of intravascular immunity is reshaping our understanding of immune surveillance, challenging the traditional view that immune responses are confined to either tissue parenchyma or the bloodstream. Our pilot study utilized intravascular staining (ivs) in rhesus macaques (RhM) to spatially distinguish pulmonary vasculature-associated (ivs+) CD8+ T cells from interstitial (ivs-) T cells. Single-cell RNA sequencing and flow cytometry revealed that ivs+ T cells are not passive blood contaminants but rather a distinct, "resident-like" population enriched in cytotoxic effectors, with elevated expression of transcripts associated with tissue residency, cell adhesion, and vascular/platelet interactions, while ivs- T cells exhibited a classic TRM signature. The presence of SIV-specific tetramer+ ivs+ CD8+ T cells in infected RhM suggests a role in antiviral defense within the lung vasculature. These findings provide new insight into intravascular immunity, highlighting a unique population of CD8+ T cells as potential pulmonary vascular sentinels poised for rapid immune responses.
© 2025 The Author(s).
Product Citations: 24
In IScience on 20 June 2025 by Melton, A., Potter, E. L., et al.
-
Cardiovascular biology
-
Immunology and Microbiology
Non-human primate model of long-COVID identifies immune associates of hyperglycemia.
In Nature Communications on 20 August 2024 by Palmer, C. S., Perdios, C., et al.
Hyperglycemia, and exacerbation of pre-existing deficits in glucose metabolism, are manifestations of the post-acute sequelae of SARS-CoV-2. Our understanding of metabolic decline after acute COVID-19 remains unclear due to the lack of animal models. Here, we report a non-human primate model of metabolic post-acute sequelae of SARS-CoV-2 using SARS-CoV-2 infected African green monkeys. Using this model, we identify a dysregulated blood chemokine signature during acute COVID-19 that correlates with elevated and persistent hyperglycemia four months post-infection. Hyperglycemia also correlates with liver glycogen levels, but there is no evidence of substantial long-term SARS-CoV-2 replication in the liver and pancreas. Finally, we report a favorable glycemic effect of the SARS-CoV-2 mRNA vaccine, administered on day 4 post-infection. Together, these data suggest that the African green monkey model exhibits important similarities to humans and can be utilized to assess therapeutic candidates to combat COVID-related metabolic defects.
© 2024. The Author(s).
-
Immunology and Microbiology
Cervical mucosal inflammation expands functional polymorphonuclear myeloid-derived suppressor cells
Preprint on MedRxiv : the Preprint Server for Health Sciences on 10 July 2024 by Pieren, D. K., Benítez-Martínez, A., et al.
The mucosal immune system plays a fundamental role in maintaining microbial balance. Microbial imbalance in the female genital tract increases the risk for adverse health outcomes in women and may increase susceptibility to genital tract infections. Among different relevant immune subsets, myeloid-derived suppressor cells (MDSCs) remain understudied in the context of female genital tract conditions. Here we show that frequency of polymorphonuclear (PMN-) MDSCs increased in the cervical mucosa of women with Chlamydia trachomatis , bacterial vaginosis, or with a coinfection, but not in women with human papillomavirus. Mucosal PMN-MDSC frequencies correlated with mucosal IL-1β in C. trachomatis patients and ex vivo exposure of cervical tissue to C. trachomatis elevated both PMN-MDSC frequencies and IL-1β secretion. Likewise, exposure of cervical tissue to cervicovaginal lavage fluid from C. trachomatis and bacterial vaginosis patients also enhanced PMN-MDSC frequencies. Lastly, cervical MDSCs expressed suppressive mediators and functionally suppressed cytotoxic T-cell responses. Our study identifies IL-1β-stimulated PMN-MDSCs as an immune suppressive mediator in female genital tract infections, potentially contributing to susceptibility to acquiring secondary infections at this site.
-
Immunology and Microbiology
In The Journal of Clinical Investigation on 15 November 2023 by Zanvit, P., van Dyk, D., et al.
Prostate cancer is generally considered an immunologically "cold" tumor type that is insensitive to immunotherapy. Targeting surface antigens on tumors through cellular therapy can induce a potent antitumor immune response to "heat up" the tumor microenvironment. However, many antigens expressed on prostate tumor cells are also found on normal tissues, potentially causing on-target, off-tumor toxicities and a suboptimal therapeutic index. Our studies revealed that six-transmembrane epithelial antigen of prostate-2 (STEAP2) was a prevalent prostate cancer antigen that displayed high, homogeneous cell surface expression across all stages of disease with limited distal normal tissue expression, making it ideal for therapeutic targeting. A multifaceted lead generation approach enabled development of an armored STEAP2 chimeric antigen receptor T cell (CAR-T) therapeutic candidate, AZD0754. This CAR-T product was armored with a dominant-negative TGF-β type II receptor, bolstering its activity in the TGF-β-rich immunosuppressive environment of prostate cancer. AZD0754 demonstrated potent and specific cytotoxicity against antigen-expressing cells in vitro despite TGF-β-rich conditions. Further, AZD0754 enforced robust, dose-dependent in vivo efficacy in STEAP2-expressing cancer cell line-derived and patient-derived xenograft mouse models, and exhibited encouraging preclinical safety. Together, these data underscore the therapeutic tractability of STEAP2 in prostate cancer as well as build confidence in the specificity, potency, and tolerability of this potentially first-in-class CAR-T therapy.
-
FC/FACS
-
Cancer Research
-
Immunology and Microbiology
In Cell Reports Medicine on 17 October 2023 by Astorga-Gamaza, A., Perea, D., et al.
Human immunodeficiency virus (HIV) infection induces immunological dysfunction, which limits the elimination of HIV-infected cells during treated infection. Identifying and targeting dysfunctional immune cells might help accelerate the purging of the persistent viral reservoir. Here, we show that chronic HIV infection increases natural killer (NK) cell populations expressing the negative immune regulator KLRG1, both in peripheral blood and lymph nodes. Antiretroviral treatment (ART) does not reestablish these functionally impaired NK populations, and the expression of KLRG1 correlates with active HIV transcription. Targeting KLRG1 with specific antibodies significantly restores the capacity of NK cells to kill HIV-infected cells, reactivates latent HIV present in CD4+ T cells co-expressing KLRG1, and reduces the intact HIV genomes in samples from ART-treated individuals. Our data support the potential use of immunotherapy against the KLRG1 receptor to impact the viral reservoir during HIV persistence.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Immunology and Microbiology
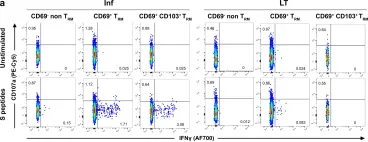
In Nat Commun on 5 April 2023 by Pieren, D. K., Kuguel, S. G., et al.
Fig.3.A

-
FC/FACS
-
Homo sapiens (Human)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 1