Cytometry by time of flight (CyTOF) is a flow cytometry-based technique using metal-tagged antibodies, allowing immunophenotyping. Here, we present a protocol for phenotyping mouse myeloid and lymphoid cells isolated from lung, spleen, and intraperitoneal lavages in healthy or pathologic conditions. We describe steps for antibody labeling and titration, tissue dissociations, and staining. We then detail procedures to compare staining obtained from fresh or cryopreserved tissues. For complete details on the use and execution of this protocol, please refer to Morin et al.1.
Copyright © 2025 The Authors. Published by Elsevier Inc. All rights reserved.
Product Citations: 30
Protocol for phenotyping mouse myeloid and lymphoid cells by mass cytometry.
In STAR Protocols on 21 March 2025 by Morin, L., Autier, B., et al.
In JCI Insight on 22 September 2021 by Luo, S., Kwon, J., et al.
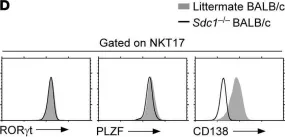
Invariant NKT (iNKT) cells are potent immunomodulatory cells that acquire effector function during their development in the thymus. IL-17-producing iNKT cells are commonly referred to as NKT17 cells, and they are unique among iNKT cells to express the heparan sulfate proteoglycan CD138 and the transcription factor RORγt. Whether and how CD138 and RORγt contribute to NKT17 cell differentiation, and whether there is an interplay between RORγt and CD138 expression to control iNKT lineage fate, remain mostly unknown. Here, we showed that CD138 expression was only associated with and not required for the differentiation and IL-17 production of NKT17 cells. Consequently, CD138-deficient mice still generated robust numbers of IL-17-producing RORγt+ NKT17 cells. Moreover, forced expression of RORγt significantly promoted the generation of thymic NKT17 cells, but did not induce CD138 expression on non-NKT17 cells. These results indicated that NKT17 cell generation and IL-17 production were driven by RORγt, employing mechanisms that were independent of CD138. Therefore, our study effectively dissociated CD138 expression from the RORγt-driven molecular pathway of NKT17 cell differentiation.
-
FC/FACS
-
Stem Cells and Developmental Biology
In Brain on 17 August 2021 by Williams, G. P., Schonhoff, A. M., et al.
α-Synuclein, a key pathological component of Parkinson's disease, has been implicated in the activation of the innate and adaptive immune system. This immune activation includes microgliosis, increased inflammatory cytokines, and the infiltration of T cells into the CNS. More recently, peripherally circulating CD4 and CD8 T cells derived from individuals with Parkinson's disease have been shown to produce Th1/Th2 cytokines in response to α-synuclein, suggesting there may be a chronic memory T cell response present in Parkinson's disease. To understand the potential effects of these α-syn associated T cell responses we used an α-synuclein overexpression mouse model, T cell-deficient mice, and a combination of immunohistochemistry and flow cytometry. In this study, we found that α-synuclein overexpression in the midbrain of mice leads to the upregulation of the major histocompatibility complex II (MHCII) protein on CNS myeloid cells as well as the infiltration of IFNγ producing CD4 and CD8 T cells into the CNS. Interestingly, genetic deletion of TCRβ or CD4, as well as the use of the immunosuppressive drug fingolimod, were able to reduce the CNS myeloid MHCII response to α-synuclein. Furthermore, we observed that CD4-deficient mice were protected from the dopaminergic cell loss observed due to α-syn overexpression. These results suggest that T cell responses associated with α-synuclein pathology may be damaging to key areas of the CNS in Parkinson's disease and that targeting these T cell responses could be an avenue for disease modifying treatments.
© The Author(s) (2021). Published by Oxford University Press on behalf of the Guarantors of Brain.
-
Immunology and Microbiology
-
Neuroscience
In Mucosal Immunology on 1 May 2021 by Takasato, Y., Kurashima, Y., et al.
Oral immunotherapy (OIT) is an effective approach to controlling food allergy. Although the detailed molecular and cellular mechanisms of OIT are unknown currently, they must be understood to advance the treatment of allergic diseases in general. To elucidate the mechanisms of OIT, especially during the immunological transition from desensitization to allergy regulation, we generated a clinical OIT murine model and used it to examine immunological events of OIT. We found that in mice that completed OIT successfully, desensitized mast cells (MCs) showed functionally beneficial alterations, such as increased induction of regulatory cytokines and enhanced expansion of regulatory T cells. Importantly, these regulatory-T-cell-mediated inhibitions of allergic responses were dramatically decreased in mice lacking OIT-induced desensitized MC. Collectively, these findings show that the desensitization process modulates the activation of MCs, leading directly to enhanced induction of regulatory-T-cell expansion and promotion of clinical allergic unresponsiveness. Our results suggest that efficiently inducing regulatory MCs is a novel strategy for the treatment of allergic disease.
-
Immunology and Microbiology
In International Journal of Environmental Research and Public Health on 25 February 2021 by Riemschneider, S., Hoffmann, M., et al.
Inflammatory bowel diseases (IBD), such as Crohn's disease and ulcerative colitis, are multifactorial inflammatory disorders of the gastrointestinal tract, characterised by abdominal cramps, bloody diarrhoea, and anaemia. Standard therapies, including corticosteroids or biologicals, often induce severe side effects, or patients may develop resistance to those therapies. Thus, new therapeutic options for IBD are urgently needed. This study investigates the therapeutic efficacy and safety of two plant-derived ligands of the aryl hydrocarbon receptor (AhR), quercetin (Q), and indol-3-carbinol (I3C), using a translationally relevant mouse model of IBD. Q and I3C are administered by gavage to C57BL/6 wild-type or C57BL/6 Ahr-/- mice suffering from chronic colitis, induced by dextran sulphate sodium (DSS). The course of the disease, intestinal histopathological changes, and in-situ immunological phenotype are scored over 25 days. Our results show that both Q and I3C improved significantly clinical symptoms in moderate DSS colitis, which coincides with a significantly reduced histopathological score. Even in severe DSS colitis I3C, neither Q nor the therapy control 6-thioguanine (6-TG) can prevent a fatal outcome. Moreover, treatment with Q or I3C restored in part DSS-induced loss of epithelial integrity by induction of tight-junction proteins and reduced significantly gut inflammation, as demonstrated by colonoscopy, as well as by immunohistochemistry revealing lower numbers of neutrophils and macrophages. Moreover, the number of Th17 cells is significantly reduced, while the number of Treg cells is significantly increased by treatment with Q or I3C, as well as 6-TG. Q- or I3C-induced amelioration of colitis is not observed in Ahr-/- mice suggesting the requirement of AhR ligation and signalling. Based on the results of this study, plant-derived non-toxic AhR agonists can be considered promising therapeutics in IBD therapy in humans. However, they may differ in terms of efficacy; therefore, it is indispensable to study the dose-response relationship of each individual AhR agonist also with regard to potential adverse effects, since they may also exert AhR-independent effects.
-
IHC
-
Immunology and Microbiology
In JCI Insight on 22 September 2021 by Luo, S., Kwon, J., et al.
Fig.2.B

-
FC/FACS
-
Collected and cropped from JCI Insight by CiteAb, provided under a CC-BY license
Image 1 of 2
In JCI Insight on 22 September 2021 by Luo, S., Kwon, J., et al.
Fig.2.D

-
FC/FACS
-
Collected and cropped from JCI Insight by CiteAb, provided under a CC-BY license
Image 1 of 2