Immunogenic cell death (ICD) and ferroptosis have recently emerged as key factors in the anticancer immune response. Among the treatments able to induce ICD and the associated release of danger signals is photodynamic therapy (PDT). Ferroptosis for its part results from lipid peroxidation and is induced by CD8+ T cells to kill nearby cancer cells on IFN-γ production. We aimed to combine the two concepts, that is, to evaluate whether the strong pro-oxidant effects of PDT may promote ferroptosis and antigen release and to develop a procedure for in situ PDT to prepare the soil for highly endocytotic immature dendritic cell (iDC) adoptive transfer. This approach was implemented for managing peritoneal carcinomatosis, a lesion often associated with poor outcomes.
We used three-dimensional (3D) heterotypic spheroids made of cancer cells, exposed them to a white light-activated OR141 photosensitizer (PS), and subsequently complexified them by adding iDC and naive lymphocytes. We next used a model of mouse peritoneal carcinomatosis and administered PDT using laparoscopy to locally induce photoactivation using the endoscope light. The immune response following adoptive transfer of iDC was tracked both in vivo and ex vivo using isolated immune cells from in situ vaccinated mice.
Cancer cells undergoing PDT-induced cell death significantly increased ICD markers and the infiltration of iDCs in spheroids, relying on ferroptosis. These actions induced the sequential activation of CD8+ and CD4+ T cells as revealed by a significant spheroid 3D structure deterioration and, remarkably, were not recapitulated by conventional ferroptosis inducer RSL3. Using LED light from an endoscope for in situ photoactivation of PS enabled us to apply the vaccination modality in mice with peritoneal tumors. Consecutive intraperitoneal injection of iDCs resulted in delayed tumor growth, increased survival rates, and prevented tumor relapse on rechallenge. CD8+ T cell response was supported by depletion experiments, nodal detection of early activated T cells, and ex vivo T cell-induced cytotoxicity toward spheroids.
The combination of in situ PDT locally delivered by an endoscope light and iDC administration induces a durable memory immune response against peritoneal carcinomatosis thereby opening new perspectives for the treatment of a life-threatening condition.
© Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Product Citations: 17
In Journal for Immunotherapy of Cancer on 5 November 2024 by Degavre, C., Lepez, A., et al.
-
Immunology and Microbiology
Targeting METTL3 reprograms the tumor microenvironment to improve cancer immunotherapy.
In Cell Chemical Biology on 18 April 2024 by Yu, H., Liu, J., et al.
The tumor microenvironment (TME) is a heterogeneous ecosystem containing cancer cells, immune cells, stromal cells, cytokines, and chemokines which together govern tumor progression and response to immunotherapies. Methyltransferase-like 3 (METTL3), a core catalytic subunit for RNA N6-methyladenosine (m6A) modification, plays a crucial role in regulating various physiological and pathological processes. Whether and how METTL3 regulates the TME and anti-tumor immunity in non-small-cell lung cancer (NSCLC) remain poorly understood. Here, we report that METTL3 elevates expression of pro-tumorigenic chemokines including CXCL1, CXCL5, and CCL20, and destabilizes PD-L1 mRNA in an m6A-dependent manner, thereby shaping a non-inflamed TME. Thus, inhibiting METTL3 reprograms a more inflamed TME that renders anti-PD-1 therapy more effective in several murine lung tumor models. Clinically, NSCLC patients who exhibit low-METTL3 expression have a better prognosis when receiving anti-PD-1 therapy. Collectively, our study highlights targeting METTL3 as a promising strategy to improve immunotherapy in NSCLC patients.
Copyright © 2023 Elsevier Ltd. All rights reserved.
-
Cancer Research
-
Immunology and Microbiology
In Cell Reports Medicine on 20 February 2024 by Wang, Q., Wang, J., et al.
Programmed cell death-1 (PD-1)/programmed cell death ligand-1 (PD-L1) blockade has become a mainstay of cancer immunotherapy. Targeting the PD-1/PD-L1 axis with small molecules is an attractive approach to enhance antitumor immunity. Here, we identified a natural marine product, benzosceptrin C (BC), that enhances the cytotoxicity of T cells to cancer cells by reducing the abundance of PD-L1. Furthermore, BC exerts its antitumor effect in mice bearing MC38 tumors by activating tumor-infiltrating T cell immunity. Mechanistic studies suggest that BC can prevent palmitoylation of PD-L1 by inhibiting DHHC3 enzymatic activity. Subsequently, PD-L1 is transferred from the membrane to the cytoplasm and cannot return to the membrane via recycling endosomes, triggering lysosome-mediated degradation of PD-L1. Moreover, the combination of BC and anti-CTLA4 effectively enhances antitumor T cell immunity. Our findings reveal a previously unrecognized antitumor mechanism of BC and represent an alternative immune checkpoint blockade (ICB) therapeutic strategy to enhance the efficacy of cancer immunotherapy.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
-
Mus musculus (House mouse)
-
Cell Biology
-
Immunology and Microbiology
ERK and USP5 govern PD-1 homeostasis via deubiquitination to modulate tumor immunotherapy.
In Nature Communications on 19 May 2023 by Xiao, X., Shi, J., et al.
The programmed cell death protein 1 (PD-1) is an inhibitory receptor on T cells and plays an important role in promoting cancer immune evasion. While ubiquitin E3 ligases regulating PD-1 stability have been reported, deubiquitinases governing PD-1 homeostasis to modulate tumor immunotherapy remain unknown. Here, we identify the ubiquitin-specific protease 5 (USP5) as a bona fide deubiquitinase for PD-1. Mechanistically, USP5 interacts with PD-1, leading to deubiquitination and stabilization of PD-1. Moreover, extracellular signal-regulated kinase (ERK) phosphorylates PD-1 at Thr234 and promotes PD-1 interaction with USP5. Conditional knockout of Usp5 in T cells increases the production of effector cytokines and retards tumor growth in mice. USP5 inhibition in combination with Trametinib or anti-CTLA-4 has an additive effect on suppressing tumor growth in mice. Together, this study describes a molecular mechanism of ERK/USP5-mediated regulation of PD-1 and identifies potential combinatorial therapeutic strategies for enhancing anti-tumor efficacy.
© 2023. The Author(s).
-
FC/FACS
-
Homo sapiens (Human)
-
Mus musculus (House mouse)
-
Cancer Research
-
Immunology and Microbiology
Preprint on Research Square on 14 March 2023 by Tsai, P., Hsu, W., et al.
Phosphatase and tensin homolog (PTEN) is a negative regulator for PI3K signaling essential for B cell development. To explore the physiological effects of PTEN mutation on peripheral B cells, we generated CD23/cre-PTEN Flox/Flox (CD23-cKO) mice in this study to avoid the developmental arrest. The mutant mice develop systemic inflammation associated with B cell expansion in the early phase followed with a severe immune cell-infiltration in multiple vital organs. PTEN deficiency leads to an accumulation of PI(3)P, an increase of lysosomal recruitment of TLR9/p38 complex, and an aberrant activation of TLR9/IL-6 axis in B cells. Interestingly, cholesterol biosynthesis pathway is upregulated in mutant cells upon TLR9 engagement. A blockade of cholesterol biosynthesis by targeting SQLE greatly reduces the level of PI(3)P and the interaction between TLR9 and p38, which lowers the level of TLR9-induced IL-6. Thus, PTEN represents a critical metabolic checkpoint that fine-tunes lipid and cholesterol homeostasis to control TLR9-driven inflammation.
-
FC/FACS
-
Mus musculus (House mouse)
-
Biochemistry and Molecular biology
-
Cell Biology
-
Immunology and Microbiology
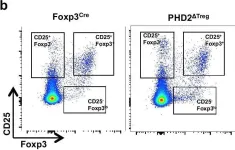
In Elife on 22 February 2022 by Ajouaou, Y., Azouz, A., et al.
Fig.2.B

-
FC/FACS
-
Mus musculus (House mouse)
Collected and cropped from Elife by CiteAb, provided under a CC-BY license
Image 1 of 1