Extracellular vesicles (EV) have emerged as promising cell-free therapeutics in regenerative medicine. However, translating primary cell line-derived EV to clinical applications requires large-scale manufacturing and several challenges, such as replicative senescence, donor heterogeneity, and genetic instability. To address these limitations, we used a reprogramming approach to generate human induced pluripotent stem cells (hiPSC) from the young source of cord blood mesenchymal stem/stromal cells (CBMSC). Capitalizing on their inexhaustible supply potential, hiPSC offer an attractive EV reservoir. Our approach encompassed an exhaustive characterization of hiPSC-EV, aligning with the rigorous MISEV2023 guidelines. Analyses demonstrated physical features compatible with small EV (sEV) and established their identity and purity. Moreover, the sEV-shuttled non-coding (nc) RNA landscape, focusing on the microRNA and circular RNA cargo, completed the molecular signature. The kinetics of the hiPSC-sEV release and cell internalization assays unveiled robust EV production and consistent uptake by human neurons. Furthermore, hiPSC-sEV demonstrated ex vivo cell tissue-protective properties. Finally, via bioinformatics, the potential involvement of the ncRNA cargo in the hiPSC-sEV biological effects was explored. This study significantly advances the understanding of pluripotent stem cell-derived EV. We propose cord blood MSC-derived hiPSC as a promising source for potentially therapeutic sEV.
© The author(s).
Product Citations: 53
In International Journal of Biological Sciences on 12 December 2024 by Barilani, M., Peli, V., et al.
-
Stem Cells and Developmental Biology
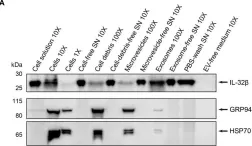
IL-2 and TCR stimulation induce expression and secretion of IL-32β by human T cells.
In Frontiers in Immunology on 31 August 2024 by Sanna, F. C., Benešová, I., et al.
IL-32 expression is important for pathogen clearance but detrimental in chronic inflammation, autoimmunity, and cancer. T cells are major IL-32 producers in these diseases and key mediators of pathogen and tumor elimination but also autoimmune destruction. However, their contribution to IL-32 biology during immune responses is hardly understood due to several isoforms with divergent inflammatory properties. Here, we identified IL-32β as the predominant isoform in various T cell subsets of healthy individuals and breast cancer patients with the highest levels detected in intratumoral regulatory T cells. We show that IL-32β is induced by IL-2 but IL-32β release requires T Cell Receptor rather than IL2R stimulation. Using inhibitors of protein secretion pathways and serial (ultra)centrifugation of T cell supernatants, we demonstrate that T cells actively secrete IL-32β unconventionally, as a free protein and, to a minor degree, through exosomes. Thus, our data identify activated T cells as major IL-32β secretors in health and cancer.
Copyright © 2024 Sanna, Benešová, Pervan, Krenz, Wurzel, Lohmayer, Mühlbauer, Wöllner, Köhl, Menevse, Stamova, Volpin, Beckhove and Xydia.
-
WB
-
Homo sapiens (Human)
-
Immunology and Microbiology
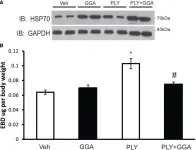
Cleavage of Hsp70.1 causes lysosomal cell death under stress conditions.
In Frontiers in Molecular Biosciences on 11 June 2024 by Yamashima, T., Mochly-Rosen, D., et al.
Autophagy mediates the degradation of intracellular macromolecules and organelles within lysosomes. There are three types of autophagy: macroautophagy, microautophagy, and chaperone-mediated autophagy. Heat shock protein 70.1 (Hsp70.1) exhibits dual functions as a chaperone protein and a lysosomal membrane stabilizer. Since chaperone-mediated autophagy participates in the recycling of ∼30% cytosolic proteins, its disorder causes cell susceptibility to stress conditions. Cargo proteins destined for degradation such as amyloid precursor protein and tau protein are trafficked by Hsp70.1 from the cytosol into lysosomes. Hsp70.1 is composed of an N-terminal nucleotide-binding domain (NBD) and a C-terminal domain that binds to cargo proteins, termed the substrate-binding domain (SBD). The NBD and SBD are connected by the interdomain linker LL1, which modulates the allosteric structure of Hsp70.1 in response to ADP/ATP binding. After the passage of the Hsp70.1-cargo complex through the lysosomal limiting membrane, high-affinity binding of the positive-charged SBD with negative-charged bis(monoacylglycero)phosphate (BMP) at the internal vesicular membranes activates acid sphingomyelinase to generate ceramide for stabilizing lysosomal membranes. As the integrity of the lysosomal limiting membrane is critical to ensure cargo protein degradation within the acidic lumen, the disintegration of the lysosomal limiting membrane is lethal to cells. After the intake of high-fat diets, however, β-oxidation of fatty acids in the mitochondria generates reactive oxygen species, which enhance the oxidation of membrane linoleic acids to produce 4-hydroxy-2-nonenal (4-HNE). In addition, 4-HNE is produced during the heating of linoleic acid-rich vegetable oils and incorporated into the body via deep-fried foods. This endogenous and exogenous 4-HNE synergically causes an increase in its serum and organ levels to induce carbonylation of Hsp70.1 at Arg469, which facilitates its conformational change and access of activated μ-calpain to LL1. Therefore, the cleavage of Hsp70.1 occurs prior to its influx into the lysosomal lumen, which leads to lysosomal membrane permeabilization/rupture. The resultant leakage of cathepsins is responsible for lysosomal cell death, which would be one of the causative factors of lifestyle-related diseases.
Copyright © 2024 Yamashima, Mochly-Rosen, Wakatsuki, Mizukoshi, Seike, Larus, Chen, Takemura, Saito and Ohashi.
-
Cell Biology
In Frontiers in Oncology on 1 May 2023 by Morimoto, M., Maishi, N., et al.
Tumor blood vessels play a key role in tumor metastasis. We have previously reported that tumor endothelial cells (TECs) exhibit abnormalities compared to normal endothelial cells. However, it is unclear how TECs acquire these abnormalities. Tumor cells secrete extracellular vesicles (EVs) to create a suitable environment for themselves. We have previously identified miR-1246 to be more abundant in high metastatic melanoma EVs than in low metastatic melanoma EVs. In the current study, we focused on miR-1246 as primarily responsible for acquiring abnormalities in TECs and examined whether the alteration of endothelial cell (EC) character by miR-1246 promotes cancer metastasis.
We analyzed the effect of miR-1246 in metastatic melanoma, A375SM-EVs, in vivo metastasis. The role of tumor EV-miR-1246 in the adhesion between ECs and tumor cells and the EC barrier was addressed. Changes in the expression of adhesion molecule and endothelial permeability were examined.
Intravenous administration of A375SM-EVs induced tumor cell colonization in the lung resulting in lung metastasis. In contrast, miR-1246 knockdown in A375SM decreased lung metastasis in vivo. miR-1246 transfection in ECs increased the expression of adhesion molecule ICAM-1 via activation of STAT3, followed by increased tumor cell adhesion to ECs. Furthermore, the expression of VE-Cadherin was downregulated in miR-1246 overexpressed EC. A375SM-EV treatment enhanced endothelial permeability. VE-Cadherin was validated as the potential target gene of miR-1246 via the target gene prediction database and 3' UTR assay.
miR-1246 in high metastatic tumor EVs promotes lung metastasis by inducing the adhesion of tumor cells to ECs and destroying the EC barrier.
Copyright © 2023 Morimoto, Maishi, Tsumita, Alam, Kikuchi, Hida, Yoshioka, Ochiya, Annan, Takeda, Kitagawa and Hida.
-
Cancer Research
In Journal of Extracellular Biology on 1 September 2022 by Hirschberg, Y., Boonen, K., et al.
Extracellular vesicles (EVs) are suggested to have a role in the progression of neurodegeneration, and are able to transmit pathological proteins from one cell to another. One of the biofluids from which EVs can be isolated is cerebrospinal fluid (CSF). However, so far, few studies have been performed on small volumes of CSF. Since pooling of patient samples possibly leads to the loss of essential individual patient information, and CSF samples are precious, it is important to have efficient techniques for the isolation of EVs from smaller volumes. In this study, the SmartSEC HT isolation kit from System Biosciences has been evaluated for this purpose. The SmartSEC HT isolation kit was used for isolation of EVs from 500 μL starting volumes of CSF, resulting in two possible EV fractions of 500 μL. Both fractions were characterised and compared to one another using a whole range of characterisation techniques. Results indicated the presence of EVs in both fractions, albeit fraction 1 showed more reproducible results over the different characterisation methods. For example, CMG (CellMask Green membrane stain) fluorescence nanotracking analysis (NTA), ExoView, and the particles/μg ratio demonstrated a clear difference between fraction 1 and 2, where fraction 1 came out as the one where most EVs were eluted with the least contamination. In the other methods, this difference was less noticeable. We successfully performed complementary characterisation tests using only 500 μL of CSF starting volume, and, conclude that fraction 1 consisted of sufficiently pure EVs for further biomarker studies. This means that future EV extractions may be based upon smaller CSF quantities, such as from individual patients. In that way, patient samples do not have to be pooled and individual patient information can be included in forthcoming studies, potentially linking EV content, size and distribution to individualised neurological diagnoses.
© 2022 The Authors. Journal of Extracellular Biology published by Wiley Periodicals, LLC on behalf of the International Society for Extracellular Vesicles.
-
Neuroscience
In Front Immunol on 31 August 2024 by Sanna, F. C., Benešová, I., et al.
Fig.8.A

-
WB
-
Homo sapiens (Human)
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 6
In Front Immunol on 29 June 2018 by Li, X., Yu, Y., et al.
Fig.7.A

-
WB
-
Collected and cropped from Front Immunol by CiteAb, provided under a CC-BY license
Image 1 of 6
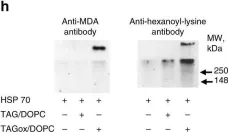
In Nat Commun on 14 December 2017 by Veglia, F., Tyurin, V. A., et al.
Fig.6.H

-
WB
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 6
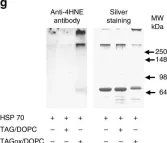
In Nat Commun on 14 December 2017 by Veglia, F., Tyurin, V. A., et al.
Fig.6.G

-
WB
-
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 6
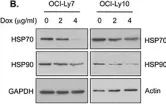
In Oncotarget on 20 June 2015 by Pulvino, M., Chen, L., et al.
Fig.7.B

-
WB
-
Homo sapiens (Human)
Collected and cropped from Oncotarget by CiteAb, provided under a CC-BY license
Image 1 of 6
In Oncotarget on 20 June 2015 by Pulvino, M., Chen, L., et al.
Fig.5.B

-
WB
-
Homo sapiens (Human)
Collected and cropped from Oncotarget by CiteAb, provided under a CC-BY license
Image 1 of 6