Transcription-replication conflicts (TRCs) induce formation of cotranscriptional RNA:DNA hybrids (R-loops) stabilized by G-quadruplexes (G4s) on the displaced DNA strand, which can cause fork stalling. Although it is known that these stalled forks can resume DNA synthesis in a process initiated by MUS81 endonuclease, how TRC-associated G4/R-loops are removed to allow fork passage remains unclear. Here, we identify the mismatch repair protein MutSβ, an MLH1-PMS1 heterodimer termed MutLβ, and the G4-resolving helicase FANCJ as factors that are required for MUS81-initiated restart of DNA replication at TRC sites in human cells. This DNA repair process depends on the G4-binding activity of MutSβ, the helicase activity of FANCJ, and the binding of FANCJ to MLH1. Furthermore, we show that MutSβ, MutLβ, and MLH1-FANCJ interaction mediate FANCJ recruitment to G4s. These data suggest that MutSβ, MutLβ, and FANCJ act in conjunction to eliminate G4/R-loops at TRC sites, allowing replication restart.
Product Citations: 30
In Science Advances on 9 February 2024 by Isik, E., Shukla, K., et al.
-
WB
-
Genetics
In NAR Cancer on 1 December 2023 by Slyskova, J., Muniesa-Vargas, A., et al.
The therapeutic efficacy of cisplatin and oxaliplatin depends on the balance between the DNA damage induction and the DNA damage response of tumor cells. Based on clinical evidence, oxaliplatin is administered to cisplatin-unresponsive cancers, but the underlying molecular causes for this tumor specificity are not clear. Hence, stratification of patients based on DNA repair profiling is not sufficiently utilized for treatment selection. Using a combination of genetic, transcriptomics and imaging approaches, we identified factors that promote global genome nucleotide excision repair (GG-NER) of DNA-platinum adducts induced by oxaliplatin, but not by cisplatin. We show that oxaliplatin-DNA lesions are a poor substrate for GG-NER initiating factor XPC and that DDB2 and HMGA2 are required for efficient binding of XPC to oxaliplatin lesions and subsequent GG-NER initiation. Loss of DDB2 and HMGA2 therefore leads to hypersensitivity to oxaliplatin but not to cisplatin. As a result, low DDB2 levels in different colon cancer cells are associated with GG-NER deficiency and oxaliplatin hypersensitivity. Finally, we show that colon cancer patients with low DDB2 levels have a better prognosis after oxaliplatin treatment than patients with high DDB2 expression. We therefore propose that DDB2 is a promising predictive marker of oxaliplatin treatment efficiency in colon cancer.
© The Author(s) 2023. Published by Oxford University Press on behalf of NAR Cancer.
-
WB
-
Genetics
In Medicine on 22 September 2023 by Kaneko, M., Nakashima, M., et al.
Although immunohistochemistry (IHC) for mismatch repair (MMR) proteins (MMR IHC) is used to identify DNA MMR status, universal screening of all patients with colorectal cancer (CRC) using a combination of both MMR IHC and genetic testing for the BRAFV600E mutation is limited in Japan. This study aimed to better understand the histopathological characteristics of CRCs, which exhibit both deficient mismatch repair (dMMR) and BRAFV600E mutation. MMR IHC of formalin-fixed paraffin-embedded tissues from tumor areas obtained from 651 patients with CRC who underwent surgical resection at Hamamatsu University Hospital (Hamamatsu, Japan) between August 2016 and March 2022 were used to evaluate MMR status, which was determined by staining for the expression of 4 MMR proteins (MLH1, MSH2, PMS2, and MSH6). All dMMR tumors were additionally evaluated for BRAFV600 mutation status via Sanger sequencing. Patient clinical characteristics (age, sex, tumor location, size, and tumor pathology) were then classified using their dMMR and BRAFV600 mutation statuses. Among the 651 patients with CRC, 58 carried tumors with dMMR, of which 52 were deficiency in MLH1 (dMLH1). Interestingly, all 16 medullary carcinomas that were analyzed showed characteristics corresponding to the presence of both dMLH1 and BRAFV600E mutation (P = .01). These results suggest that colorectal medullary carcinomas can be diagnosed based on their unique characteristics of harboring the BRAFV600E mutation and exhibiting dMLH1 expression.
Copyright © 2023 the Author(s). Published by Wolters Kluwer Health, Inc.
-
IHC
-
Homo sapiens (Human)
-
Cancer Research
BK Polyomavirus Requires the Mismatch Repair Pathway for DNA Damage Response Activation.
In Journal of Virology on 27 April 2022 by Justice, J. L., Needham, J. M., et al.
BK polyomavirus (PyV) infects the genitourinary tract of >90% of the adult population. Immunosuppression increases the risk of viral reactivation, making BKPyV a leading cause of graft failure in kidney transplant recipients. Polyomaviruses have a small double-stranded DNA (dsDNA) genome that requires host replication machinery to amplify the viral genome. Specifically, polyomaviruses promote S phase entry and delay S phase exit by activating the DNA damage response (DDR) pathway via an uncharacterized mechanism requiring viral replication. BKPyV infection elevates expression of MutSα, a mismatch repair (MMR) pathway protein complex that senses and repairs DNA mismatches and can activate the DDR. Thus, we investigated the role of the MMR pathway by silencing the MutSα component, Msh6, in BKPyV-infected primary cells. This resulted in severe DNA damage that correlated with weak DNA damage response activation and a failure to arrest the cell cycle to prevent mitotic entry during infection. Furthermore, silencing Msh6 expression resulted in significantly fewer infectious viral particles due to significantly lower levels of VP2, a minor capsid protein important for trafficking during subsequent infections. Since viral assembly occurs in the nucleus, our findings are consistent with a model in which entry into mitosis disrupts viral assembly due to nuclear envelope breakdown, which disperses VP2 throughout the cell, reducing its availability for encapsidation into viral particles. Thus, the MMR pathway may be required to activate the ATR (ATM-Rad3-related) pathway during infection to maintain a favorable environment for both viral replication and assembly. IMPORTANCE Since there are no therapeutics that target BKPyV reactivation in organ transplant patients, it is currently treated by decreasing immunosuppression to allow the natural immune system to fight the viral infection. Antivirals would significantly improve patient outcomes since reducing immunosuppression carries the risk of graft failure. PyVs activate the DDR, for which there are several promising inhibitors. However, a better understanding of how PyVs activate the DDR and what role the DDR plays during infection is needed. Here, we show that a component of the mismatch repair pathway is required for DDR activation during PyV infection. These findings show that the mismatch repair pathway is important for DDR activation during PyV infection and that inhibiting the DDR reduces viral titers by generating less infectious virions that lack the minor capsid protein VP2, which is important for viral trafficking.
-
WB
-
Genetics
-
Immunology and Microbiology
In Cell Reports on 31 August 2021 by Goold, R., Hamilton, J., et al.
CAG repeat expansion in the HTT gene drives Huntington's disease (HD) pathogenesis and is modulated by DNA damage repair pathways. In this context, the interaction between FAN1, a DNA-structure-specific nuclease, and MLH1, member of the DNA mismatch repair pathway (MMR), is not defined. Here, we identify a highly conserved SPYF motif at the N terminus of FAN1 that binds to MLH1. Our data support a model where FAN1 has two distinct functions to stabilize CAG repeats. On one hand, it binds MLH1 to restrict its recruitment by MSH3, thus inhibiting the assembly of a functional MMR complex that would otherwise promote CAG repeat expansion. On the other hand, it promotes accurate repair via its nuclease activity. These data highlight a potential avenue for HD therapeutics in attenuating somatic expansion.
Copyright © 2021 The Author(s). Published by Elsevier Inc. All rights reserved.
In Nat Commun on 26 August 2021 by Huang, X., Park, K. M., et al.
Fig.1.D

-
WB
-
Homo sapiens (Human)
Collected and cropped from Nat Commun by CiteAb, provided under a CC-BY license
Image 1 of 3
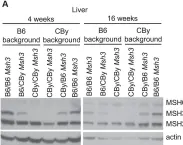
In PLoS Genet on 8 March 2013 by Tomé, S., Manley, K., et al.
Fig.3.A

-
WB
-
Collected and cropped from PLoS Genet by CiteAb, provided under a CC-BY license
Image 1 of 3
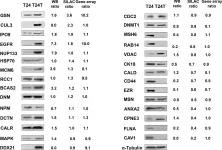
In PLoS One on 12 January 2013 by Grau, L., Luque-Garcia, J. L., et al.
Fig.3.A

-
WB
-
Homo sapiens (Human)
Collected and cropped from PLoS One by CiteAb, provided under a CC-BY license
Image 1 of 3