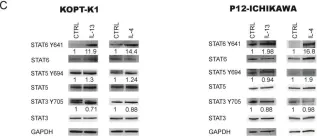
Lymphoblastic lymphoma (LBL) is the second most common type of non-Hodgkin lymphoma in childhood, mainly of T cell origin (T-LBL). Although current treatment protocols allow a complete remission in 85% of cases, the second-line treatment overall survival for patients with progressive or relapsed disease is around 14%, making this the major issue to be confronted. Thus, we performed a Reverse Phase Protein Array study in a cohort of 22 T-LBL patients to find reliable disease risk marker(s) and new therapeutic targets to improve pediatric T-LBL patients' outcome. Interestingly, we pinpointed JAK2 Y1007-1008 as a potential prognosis marker as well as a therapeutic target in poor prognosis patients. Hence, the hyperactivation of the JAK1/2-STAT6 pathway characterizes these latter patients. Moreover, we functionally demonstrated that STAT6 hyperactivation contributes to therapy resistance by binding the glucocorticoid receptor, thus inhibiting its transcriptional activity. This was further confirmed by specific STAT6 gene silencing followed by dexamethasone treatment. Finally, JAK1/2-STAT6 pathway inhibition by ruxolitinib, an FDA approved drug, in cell line models and in one T-LBL primary sample led to cell proliferation reduction and increased apoptosis. Globally, our results identify a new potential prognostic marker and suggest a novel therapeutic approach to overcome therapy resistance in pediatric T-LBL patients.
Product Citations: 7
Ruxolitinib as a Novel Therapeutic Option for Poor Prognosis T-LBL Pediatric Patients.
In Cancers on 24 July 2021 by Veltri, G., Silvestri, C., et al.
-
IP
-
WB
-
Homo sapiens (Human)
-
Cancer Research
In The Journal of Immunology on 1 November 2019 by Wu, Y., Konaté, M. M., et al.
Dual oxidase 2 (DUOX2) generates H2O2 that plays a critical role in both host defense and chronic inflammation. Previously, we demonstrated that the proinflammatory mediators IFN-γ and LPS enhance expression of DUOX2 and its maturation factor DUOXA2 through STAT1- and NF-κB‒mediated signaling in human pancreatic cancer cells. Using a panel of colon and pancreatic cancer cell lines, we now report the induction of DUOX2/DUOXA2 mRNA and protein expression by the TH2 cytokine IL-4. IL-4 activated STAT6 signaling that, when silenced, significantly decreased induction of DUOX2. Furthermore, the TH17 cytokine IL-17A combined synergistically with IL-4 to increase DUOX2 expression in both colon and pancreatic cancer cells mediated, at least in part, by signaling through NF-κB. The upregulation of DUOX2 was associated with a significant increase in the production of extracellular H2O2 and DNA damage-as indicated by the accumulation of 8-oxo-dG and γH2AX-which was suppressed by the NADPH oxidase inhibitor diphenylene iodonium and a DUOX2-specific small interfering RNA. The clinical relevance of these experiments is suggested by immunohistochemical, microarray, and quantitative RT-PCR studies of human colon and pancreatic tumors demonstrating significantly higher DUOX2, IL-4R, and IL-17RA expression in tumors than in adjacent normal tissues; in pancreatic adenocarcinoma, increased DUOX2 expression is adversely associated with overall patient survival. These data suggest a functional association between DUOX2-mediated H2O2 production and induced DNA damage in gastrointestinal malignancies.
-
WB
-
Homo sapiens (Human)
-
Cancer Research
-
Genetics
-
Immunology and Microbiology
In Cell Reports on 25 June 2019 by Chowdhury, D., Alrefai, H., et al.
Alternatively activated (M2) macrophages promote wound healing but weaken antimicrobial defenses. The mechanisms that enforce macrophage divergence and dictate the phenotypic and metabolic characteristics of M2 macrophages remain elusive. We show that alternative activation with interleukin (IL)-4 induces expression of metallothionein 3 (MT3) that regulates macrophage polarization and function. MT3 was requisite for metabolic reprograming in IL-4-stimulated macrophages or M(IL-4) macrophages to promote mitochondrial respiration and suppress glycolysis. MT3 fostered an M(IL-4) phenotype, suppressed hypoxia inducible factor (HIF)1α activation, and thwarted the emergence of a proinflammatory M1 program in macrophages. MT3 deficiency augmented macrophage plasticity, resulting in enhanced interferon γ (IFNγ) responsiveness and a dampened M(IL-4) phenotype. Thus, MT3 programs the phenotype and metabolic fate of M(IL-4) macrophages.Published by Elsevier Inc.
-
Biochemistry and Molecular biology
-
Cell Biology
In Oncotarget on 13 June 2017 by Liu, H., Antony, S., et al.
Human colon cancers express higher levels of NADPH oxidase 1 [NOX1] than adjacent normal epithelium. It has been suggested that reactive oxygen species [ROS] derived from NOX1 contribute to DNA damage and neoplastic transformation in the colon, particularly during chronic inflammatory stress. However, the mechanism(s) underlying increased NOX1 expression in malignant tumors or chronic inflammatory states involving the intestine are poorly characterized. We examined the effects of two pro-inflammatory cytokines, IL-4 and IL-13, on the regulation of NOX1. NOX1 expression was increased 4- to 5-fold in a time- and concentration-dependent manner by both cytokines in human colon cancer cell lines when a functional Type II IL-4 receptor was present. Increased NOX1 transcription following IL-4/IL-13 exposure was mediated by JAK1/STAT6 signaling, was associated with a ROS-related inhibition of protein tyrosine phosphatase activity, and was dependent upon activation and specific binding of GATA3 to the NOX1 promoter. NOX1-mediated ROS production increased cell cycle progression through S-phase leading to a significant increase in cellular proliferation. Evaluation of twenty pairs of surgically-resected colon cancers and their associated uninvolved adjacent colonic epithelium demonstrated a significant increase in the active form of NOX1, NOX1-L, in tumors compared to normal tissues, and a significant correlation between the expression levels of NOX1 and the Type II IL-4 receptor in tumor and the uninvolved colon. These studies imply that NOX1 expression, mediated by IL-4/IL-13, could contribute to an oxidant milieu capable of supporting the initiation or progression of colonic cancer, suggesting a role for NOX1 as a therapeutic target.
-
Cancer Research
In Autophagy on 24 September 2015 by Botbol, Y., Patel, B., et al.
Macroautophagy is a cellular process that mediates degradation in the lysosome of cytoplasmic components including proteins and organelles. Previous studies have shown that macroautophagy is induced in activated T cells to regulate organelle homeostasis and the cell's energy metabolism. However, the signaling pathways that initiate and regulate activation-induced macroautophagy in T cells have not been identified. Here, we show that activation-induced macroautophagy in T cells depends on signaling from common γ-chain cytokines. Consequently, inhibition of signaling through JAK3, induced downstream of cytokine receptors containing the common γ-chain, prevents full induction of macroautophagy in activated T cells. Moreover, we found that common γ-chain cytokines are not only required for macroautophagy upregulation during T cell activation but can themselves induce macroautophagy. Our data also show that macroautophagy induction in T cells is associated with an increase of LC3 expression that is mediated by a post-transcriptional mechanism. Overall, our findings unveiled a new role for common γ-chain cytokines as a molecular link between autophagy induction and T-cell activation.
-
WB
-
Mus musculus (House mouse)
-
Cell Biology
-
Immunology and Microbiology
In Cancers (Basel) on 24 July 2021 by Veltri, G., Silvestri, C., et al.
Fig.2.C

-
WB
-
Collected and cropped from Cancers (Basel) by CiteAb, provided under a CC-BY license
Image 1 of 2
In Respir Res on 15 February 2015 by Xu, J., Singhera, G. K., et al.
Fig.5.C

-
WB
-
Homo sapiens (Human)
Collected and cropped from Respir Res by CiteAb, provided under a CC-BY license
Image 1 of 2