The cytokine interleukin-6 (IL-6) plays a crucial role in autoimmune and inflammatory diseases. Understanding the precise mechanism of IL-6 interaction at the amino acid level is essential to develop IL-6-inhibiting compounds. In this study, we employed computer-guided drug design tools to predict the key residues that are involved in the interaction between IL-6 and its receptor IL-6R. Subsequently, we generated IL-6 mutants and evaluated their binding affinity to IL-6R and the IL-6R - gp130 complex, as well as monitoring their biological activities. Our findings revealed that the R167A mutant exhibited increased affinity for IL-6R, leading to enhanced binding to IL-6R - gp130 complex and subsequently elevated intracellular phosphorylation of STAT3 in effector cells. On the other hand, although E171A reduced its affinity for IL-6R, it displayed stronger binding to the IL-6R - gp130 complex, thereby enhancing its biological activity. Furthermore, we identified the importance of R178 and R181 for the precise recognition of IL-6 by IL-6R. Mutants R181A/V failed to bind to IL-6R, while maintaining an affinity for the IL-6 - gp130 complex. Additionally, deletion of the D helix resulted in complete loss of IL-6 binding affinity for IL-6R. Overall, this study provides valuable insights into the binding mechanism of IL-6 and establishes a solid foundation for future design of novel IL-6 inhibitors.
© 2024. The Author(s).
Product Citations: 56
In Scientific Reports on 7 August 2024 by Li, K., Cai, J., et al.
-
Homo sapiens (Human)
In Journal of Autoimmunity on 1 June 2024 by Esen, I., Sandovici, M., et al.
The IL-12-IFNγ-Th1 and the IL-6-IL-23-Th17 axes are considered the dominant pathogenic pathways in Giant Cell Arteritis (GCA). Both pathways signal via activation of the downstream JAK/STAT proteins. We hypothesized that phosphorylated STAT (pSTAT) signatures in circulating immune cells may aid to stratify GCA-patients for personalized treatment.
To investigate pSTAT expression, PBMCs from treatment-naive GCA-patients (n = 18), infection controls (INF, n = 11) and age-matched healthy controls (HC, n = 15) were stimulated in vitro with IL-6, IL-2, IL-10, IFN-γ, M-CSF or GM-CSF, and stained with CD3, CD4, CD19, CD45RO, pSTAT1, pSTAT3, pSTAT5 antibodies, and analyzed by flow cytometry. Serum IL-6, sIL-6-receptor and gp130 were measured by Luminex. The change in percentages of pSTAT3+CD4+T-cells was evaluated at diagnosis and at 3 months and 1-year of follow-up. Kaplan-Meier analyses was used to asses prognostic accuracy.
Analysis of IL-6 stimulated immune cell subsets revealed a significant decrease in percentages of pSTAT3+CD4+T-cells of GCA-patients and INF-controls compared to HCs. Following patient stratification according to high (median>1.5 pg/mL) and low (median<1.5 pg/mL) IL-6 levels, we observed a reduction in the pSTAT3 response in GCA-patients with high serum IL-6. Percentages of pSTAT3+CD4+T-cells in patients with high serum IL-6 levels at diagnosis normalized after glucocorticoid (GC) treatment. Importantly, we found that patients with low percentages of pSTAT3+CD4+T-cells at baseline require longer GC-treatment.
Overall, in GCA, the percentages of in vitro IL-6-induced pSTAT3+CD4+T-cells likely reflect prior in vivo exposure to high IL-6 and may serve as a prognostic marker for GC-treatment duration and may assist improving personalized treatment options in the future.
Copyright © 2024 The Authors. Published by Elsevier Ltd.. All rights reserved.
-
Homo sapiens (Human)
-
Immunology and Microbiology
Sphingolipid biosynthesis is essential for metabolic rewiring during TH17 cell differentiation.
In Science Advances on 26 April 2024 by Abimannan, T., Parthibane, V., et al.
T helper 17 (TH17) cells are implicated in autoimmune diseases, and several metabolic processes are shown to be important for their development and function. In this study, we report an essential role for sphingolipids synthesized through the de novo pathway in TH17 cell development. Deficiency of SPTLC1, a major subunit of serine palmitoyl transferase enzyme complex that catalyzes the first and rate-limiting step of de novo sphingolipid synthesis, impaired glycolysis in differentiating TH17 cells by increasing intracellular reactive oxygen species (ROS) through enhancement of nicotinamide adenine dinucleotide phosphate oxidase 2 activity. Increased ROS leads to impaired activation of mammalian target of rapamycin C1 and reduced expression of hypoxia-inducible factor 1-alpha and c-Myc-induced glycolytic genes. SPTLCI deficiency protected mice from developing experimental autoimmune encephalomyelitis and experimental T cell transfer colitis. Our results thus show a critical role for de novo sphingolipid biosynthetic pathway in shaping adaptive immune responses with implications in autoimmune diseases.
-
Biochemistry and Molecular biology
-
Cell Biology
TREM-2 Drives Development of Multiple Sclerosis by Promoting Pathogenic Th17 Polarization.
In Neuroscience Bulletin on 1 January 2024 by Qu, S., Hu, S., et al.
Multiple sclerosis (MS) is a neuroinflammatory demyelinating disease, mediated by pathogenic T helper 17 (Th17) cells. However, the therapeutic effect is accompanied by the fluctuation of the proportion and function of Th17 cells, which prompted us to find the key regulator of Th17 differentiation in MS. Here, we demonstrated that the triggering receptor expressed on myeloid cells 2 (TREM-2), a modulator of pattern recognition receptors on innate immune cells, was highly expressed on pathogenic CD4-positive T lymphocyte (CD4+ T) cells in both patients with MS and experimental autoimmune encephalomyelitis (EAE) mouse models. Conditional knockout of Trem-2 in CD4+ T cells significantly alleviated the disease activity and reduced Th17 cell infiltration, activation, differentiation, and inflammatory cytokine production and secretion in EAE mice. Furthermore, with Trem-2 knockout in vivo experiments and in vitro inhibitor assays, the TREM-2/zeta-chain associated protein kinase 70 (ZAP70)/signal transducer and activator of transcription 3 (STAT3) signal axis was essential for Th17 activation and differentiation in EAE progression. In conclusion, TREM-2 is a key regulator of pathogenic Th17 in EAE mice, and this sheds new light on the potential of this therapeutic target for MS.
© 2023. Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Sciences.
Human MCTS1-dependent translation of JAK2 is essential for IFN-γ immunity to mycobacteria.
In Cell on 9 November 2023 by Bohlen, J., Zhou, Q., et al.
Human inherited disorders of interferon-gamma (IFN-γ) immunity underlie severe mycobacterial diseases. We report X-linked recessive MCTS1 deficiency in men with mycobacterial disease from kindreds of different ancestries (from China, Finland, Iran, and Saudi Arabia). Complete deficiency of this translation re-initiation factor impairs the translation of a subset of proteins, including the kinase JAK2 in all cell types tested, including T lymphocytes and phagocytes. JAK2 expression is sufficiently low to impair cellular responses to interleukin-23 (IL-23) and partially IL-12, but not other JAK2-dependent cytokines. Defective responses to IL-23 preferentially impair the production of IFN-γ by innate-like adaptive mucosal-associated invariant T cells (MAIT) and γδ T lymphocytes upon mycobacterial challenge. Surprisingly, the lack of MCTS1-dependent translation re-initiation and ribosome recycling seems to be otherwise physiologically redundant in these patients. These findings suggest that X-linked recessive human MCTS1 deficiency underlies isolated mycobacterial disease by impairing JAK2 translation in innate-like adaptive T lymphocytes, thereby impairing the IL-23-dependent induction of IFN-γ.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
-
FC/FACS
-
Biochemistry and Molecular biology
-
Immunology and Microbiology
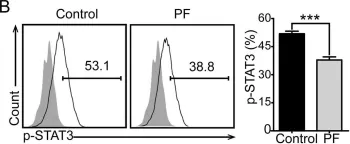
In Sci Rep on 6 February 2017 by Zhang, H., Qi, Y., et al.
Fig.4.B

-
FC/FACS
-
Collected and cropped from Sci Rep by CiteAb, provided under a CC-BY license
Image 1 of 1